Patología anal en el consultorio: un enfoque sindrómico para el diagnóstico
DOI:
https://doi.org/10.52787/agl.v54i3.429Palabras clave:
Patología anal, hemorroides, condilomas, absceso anal, proctología, diagnóstico, tratamientoResumen
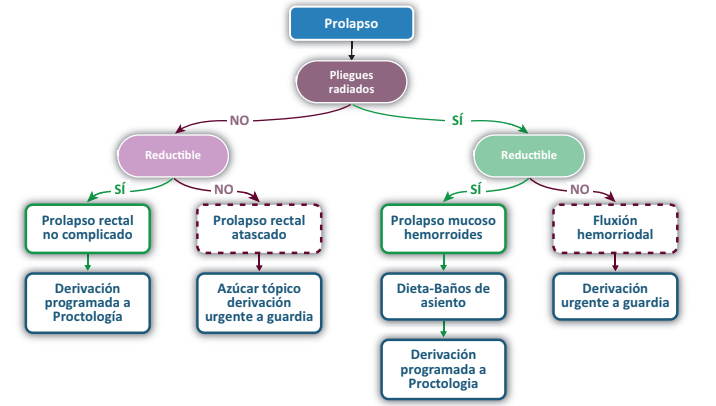
Las patologías anales representan un motivo común de consulta en la práctica médica general y especializada, y frecuentemente son mal interpretadas por los pacientes como hemorroides. Este artículo de revisión se centra en ofrecer una guía para el diagnóstico y el manejo inicial de las principales patologías anales con el propósito de asistir a médicos generales y a gastroenterólogos en su práctica diaria. En él se exploran los diagnósticos diferenciales de los síndromes más prevalentes, incluyendo el síndrome de tumor anal, el prolapso y el doloroso, y se enfatiza la importancia de una anamnesis detallada y un examen físico dirigido. El artículo además describe en detalle las características clínicas y el manejo de condiciones como plicomas, condilomas, hemorroides y abscesos anales. En el texto se discuten brevemente las opciones terapéuticas. Esta revisión proporciona herramientas prácticas para mejorar la precisión diagnóstica y la efectividad del tratamiento.
Citas
-1. Abramowitz L, Benabderrahmane M, Pospait D, Philip J, Laouénan C. The prevalence of proctological symptoms amongst patients who see general practitioners in France. European Journal of General Practice [Internet]. 2014 Apr 4;20(4):301-6. Available from: http://dx.doi.org/10.3109/13814788.2014.899578
-2. Idrees JJ, Clapp M, Brady JT, Stein SL, Reynolds HL, Steinhagen E. Evaluating the Accuracy of Hemorrhoids: Comparison Among Specialties and Symptoms. Diseases of the Colon & Rectum [Internet]. 2019 Jul;62(7):867-71. Available from: http://dx.doi.org/10.1097/DCR.0000000000001315
-3. Safer MA, Tharps QJ, Jackson TC, Levknthal H. Determinants of Three Stages of Delay in Seeking Care at a Medical Clinic. Medical Care [Internet]. 1979 Jan;17(1):11-29. Available from: http://dx.doi.org/10.1097/00005650-197901000-00002
-4. Palefsky JM, Lee JY, Jay N, Goldstone SE, Darragh TM, Dunlevy HA, et al. Treatment of Anal High-Grade Squamous Intraepithelial Lesions to Prevent Anal Cancer. New England Journal of Medicine [Internet]. 2022 Jun 16;386(24):2273-82. Available from: http://dx.doi.org/10.1056/NEJMoa2201048
-5. Wald A, Bharucha AE, Limketkai B, Malcolm A, Remes-Troche JM, Whitehead WE, et al. ACG Clinical Guidelines: Management of Benign Anorectal Disorders. American Journal of Gastroenterology [Internet]. 2021 Oct;116(10):1987-2008. Available from: http://dx.doi.org/10.14309/ajg.0000000000001507
-6. Giannini I, Amato A, Basso L, Tricomi N, Marranci M, Pecorella G, et al. Flavonoids mixture (diosmin, troxerutin, hesperidin) in the treatment of acute hemorrhoidal disease: a prospective, randomized, triple-blind, controlled trial. Techniques in Coloproctology [Internet]. 2015 Apr 19;19(6):339-45. Available from: http://dx.doi.org/10.1007/s10151-015-1302-9
-7. MacRae HM, McLeod RS. Comparison of hemorrhoidal treatment modalities. Diseases of the Colon & Rectum [Internet]. 1995 Jul;38(7):68794. Available from: http://dx.doi.org/10.1007/BF02048023
-8. Bordeianou L, Hicks CW, Kaiser AM, Alavi K, Sudan R, Wise PE. Rectal Prolapse: An Overview of Clinical Features, Diagnosis, and Patient-Specific Management Strategies. Journal of Gastrointestinal Surgery [Internet]. 2014 May;18(5):1059-69. Available from: http://dx.doi.org/10.1007/s11605-013-2427-7
-9. Pellino G, Fuschillo G, Simillis C, Selvaggi L, Signoriello G, Vinci D, et al. Abdominal versus perineal approach for external rectal prolapse: systematic review with meta-analysis. BJS Open [Internet]. 2022 Mar 8;6(2). Available from: http://dx.doi.org/10.1093/bjsopen/zrac018
-10. Brazzelli M, Bachoo P, Grant A. Surgery for complete rectal prolapse in adults. Brazzelli M, editor. 1999 Oct 25; Available from: http://dx.doi.org/10.1002/14651858.CD001758
-11. Matttacheo A, Grecco AM. Nociones de Proctología: Para médicos generales. Primera. Editores Argentinos; 2020.
-12. Selvaggi L, Sciaudone G, Canonico S, Selvaggi F, Pellino G. The Management of Acute Hemorrhoidal Disease. Reviews on Recent Clinical Trials [Internet]. 2021 Feb 15;16(1):91-5. Available from: http://dx.doi.org/10.2174/1574887115666200330162537
-13. Salati SA. Anal fissure an extensive update. Polish Journal of Surgery [Internet]. 2021 Mar 12;93(3):1-5. Available from: http://dx.doi.org/10.5604/01.3001.0014.7879
-14. Brisinda G, Maria G, Bentivoglio AR, Cassetta E, Gui D, Albanese A. A Comparison of Injections of Botulinum Toxin and Topical Nitroglycerin Ointment for the Treatment of Chronic Anal Fissure. New England Journal of Medicine [Internet]. 1999 Jul 8;341(2):65-9. Available from: http://dx.doi.org/10.1056/NEJM199907083410201
-15. Lin JX, Krishna S, Su’a B, Hill AG. Optimal Dosing of Botulinum Toxin for Treatment of Chronic Anal Fissure: A Systematic Review and Meta-Analysis. Diseases of the Colon & Rectum [Internet]. 2016 Sep;59(9):886-94. Available from: http://dx.doi.org/10.1097/DCR.0000000000000612
-16. Elsebae MMA. A Study of Fecal Incontinence in Patients with Chronic Anal Fissure: Prospective, Randomized, Controlled Trial of the Extent of Internal Anal Sphincter Division During Lateral Sphincterotomy. World Journal of Surgery [Internet]. 2007 Aug;31(10):2052-7. Available from: http://dx.doi.org/10.1007/s00268-007-9177-1
-17. Murad-Regadas SM, Fernandes GO da S, Regadas FSP, Rodrigues LV, Pereira J de JR, Regadas Filho FSP, et al. How Much of the Internal Sphincter May Be Divided During Lateral Sphincterotomy for Chronic Anal Fissure in Women? Morphologic and Functional Evaluation After Sphincterotomy. Diseases of the Colon & Rectum [Internet]. 2013 May;56(5):645-51. Available from: http://dx.doi.org/10.1097/DCR.0b013e31827a7416
-18. Lohsiriwat V. Treatment of hemorrhoids: A coloproctologist’s view. World Journal of Gastroenterology [Internet]. 2015;21(31):9245. Available from: http://dx.doi.org/10.3748/wjg.v21.i31.9245
-19. Ommer A, Herold A, Berg E, Fürst A, Post S, Ruppert R, et al. German S3 guidelines: anal abscess and fistula (second revised version). Langenbeck’s Archives of Surgery [Internet]. 2017 Mar;402(2):191–201. Available from: http://dx.doi.org/10.1007/s00423-017-1563-z
-20. Ortega AE, Bubbers E, Liu W, Cologne KG, Ault GT. A Novel Classification, Evaluation, and Treatment Strategy for Supralevator Abscesses. Diseases of the Colon & Rectum [Internet]. 2015 Nov;58(11):1109-10. Available from: http://dx.doi.org/10.1097/DCR.0000000000000468
-21. Hämäläinen KPJ, Sainio PA. Incidence of fistulas after drainage of acute anorectal abscesses. Diseases of the Colon & Rectum [Internet]. 1998 Nov;41(11):1357-61. Available from: http://dx.doi.org/10.1007/BF02237048
-22. Vincent C. Anorectal Pain and Irritation. Primary Care: Clinics in Office Practice [Internet]. 1999 Mar;26(1):53-68. Available from: http://dx.doi.org/10.1016/S0095-4543(05)70101-9
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2024 Alejandro Moreira

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.












