Nasogallbladder Drainage: Endoscopic Alternative for Severe Acute Cholecystitis
DOI:
https://doi.org/10.52787/agl.v52i2.159Keywords:
Severe acute cholecystitis, nasogallbladder drainage, high-risk patientsAbstract
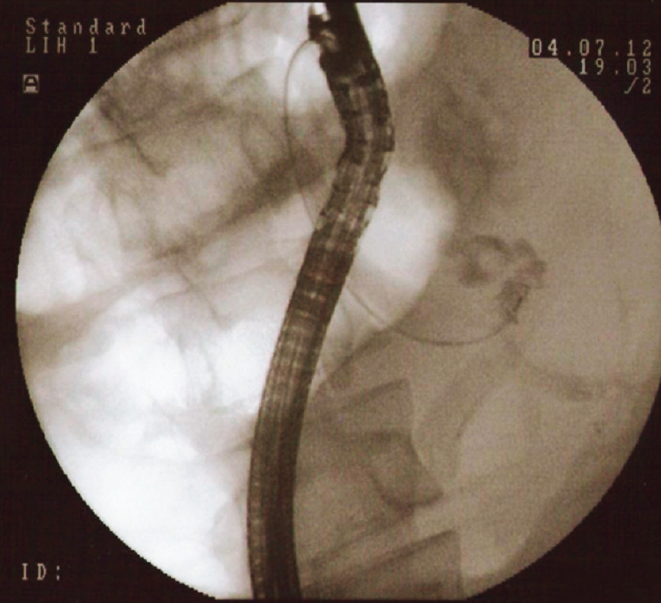
Acute cholecystitis is mainly caused by the obstruction of the cystic duct or the gallbladder neck by stones. The usual management is emergency or urgent cholecystectomy, depending on the severity of the disease. In patients at high surgical risk, gallbladder drainage is chosen, which is traditionally approached percutaneosly or with endoscopic methods through the placement of nasobiliary tubes, transpapillary stents or transmural stents by endoscopic ultrasound. The endoscopic approach has the advantage of maintaining the integrity of the skin barrier, is less painful and has less impact on the patient’s quality of life. Two clinical cases of endoscopic drainage are presented: that of a young woman with acute cholecystitis and septic shock in the context of severe burns, and that of an elderly man with similar clinical deterioration, both of whom underwent endoscopic drainage with placement of a nasogallbladder tube, with good clinical response and subsequent surgical resolution.
References
-1. Tokyo guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis. Jhbps. 2018;25(1):41-54.
-2. Bundy J, et al. Percutaneous cholecystostomy: long-term outcomes in 324 patients. Cardiovasc Intervent Radiol. 2018;41(6):928-34.
-3. Kozarek RA. Selective cannulation of the cystic duct at time of ERCP. J Clin Gastroenterol. 1984;6:37-40.
-4. Sobani Z, Ling C, Rustagi T. Endoscopic Transpapillary Gallbladder Drainage for AcuteCholecystitis. Digestive Diseases and Sciences. 2021;66:1425-35.
-5. Khan MA, Atiq O, Kubiliun N, et al. Eficacy and safety of endoscopic gallbladder drainage in acute cholecystitis: is it better than percutaneous gallbladder drainage? Gastrointest Endosc. 2017;85(1):76-87.
-6. Mohan BP, Khan SR, Trakroo S, et al. Endoscopic ultrasound-guided gallbladder drainage, transpapillary drainage, or percutaneous drainage in high risk acute cholecystitis patients: a systematic review and comparative meta-analysis. Endoscopy. 2020;52(2):96-106.
-7. Mutignani M, Iacopini F, Perri V, et al. Endoscopic gallbladder drainage for acute cholecystitis: technical and clinical results. Endoscopy. 2009;41:539-46.
-8. Kaura K, Bazerbachi F, Sawas T, et al. Surgical outcomes of ERCP-guided transpapillary gallbladder drainage versus percutaneous cholecystostomy as bridging therapies for acute cholecystitis followed by interval cholecystectomy. HPB (Oxford) 2019. Disponible en: https://doi.org/10.1016/j.hpb.2019.10.1530
-9. Saumoy M, Tyberg A, Brown E, et al. Successful cholecystectomy after endoscopic ultrasound gallbladder drainage compared with percutaneous cholecystostomy, can it be done? J Clin Gastroenterol. 2019;53:231-5.
-10. Xiaoping S, Yiting L, Ging H, Xuyang Z, Xingjie L, Zhiping W. Endoscopic transpapillary gallbladder drainage for management of acute cholecystitis with coagulopathy.Journal of International Medical Research. 2021;49(3):1-6.
-11. Hamada T, Yasunaga H, Nakai Y, et al. Severe bleeding after percutaneous transhepatic drainage of the biliary system: effect of antithrombotic agents-analysis of 34 606 cases from a Japanese nationwide administrative database. Radiology. 2015;274:605-13.
-12. Maruta A, Iwata K, Iwashita T, Mizoguchi K, Kimura M, Takeyama H, Joh T. Factors affecting technical success of endoscopic transpapillary gallbladder drainage for acute cholecystitis. J. Hepato-Biliary-Pancreat. Sci. 2020;27:429-36.
-13. Thomas R, McCarty KE Hathorn, ANB, Kunal J, Marvin R, Christopher C Thompson. Endoscopic gallbladder drainage for symptomatic gallbladder disease: a cumulative systematic review meta‑analysis. Surgical Endoscopy. 2021;35:4964-85.
-14. Khan MA, Atiq O, Kubiliun N, Ali B, Kamal F, Nollan R, et al. Efficacy and safety of endoscopic gallbladder drainage in acute cholecystitis: is it better than percutaneous gallbladder drainage? Gastrointest Endosc. 2017;85:76-87.
-15. Saumoy M, Yang J, Bhatt A, Bucobo J, Chandrasekhara V, Copland A, Krishnan K, Law R, Pannala R, Parsi M, Rahimi M, Trikudanathan G, Trindade A, LichtensteinD. ASGE. Endoscopic therapies for gallbladder drainage. GIE. 2021;94:671-84.
-16. Sobani ZA, Ling, C, Rustagi T. Endoscopic Ultrasound-Guided Gallbladder Drainage. Dig Dis Sci. 2021;66:2154-61. Disponible en: https://doi.org/10.1007/s10620-020-06520-y
-17. Lisotti A, Linguerri R, Bacchilega I, et al. EUS-guided gallbladder drainage in high-risk surgical patients with acute cholecystitis-procedure outcomes and evaluation of mortality predictors. Surg Endosc. 2022;36:569-78. Disponible en: https://doi.org/10.1007/s00464-021-08318-z
-18. Kalva NR, Vanar V, Forcione D, Bechtold ML, Puli SR. Efficacy and Safety of Lumen Apposing Self-Expandable Metal Stents for EUS Guided Cholecystostomy: A Meta-Analysis and Systematic Review. Can J Gastroenterol Hepatol. 2018 Apr 12;2018:7070961. doi: 10.1155/2018/7070961PMID: 29850458; PMCID: PMC5925026.
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Daniela Caamaño, Carolina Dutto, José Adi

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.












