Abordaje del paciente con dolor torácico no cardiogénico de origen esofágico
DOI:
https://doi.org/10.52787/agl.v52i4.276Palabras clave:
Dolor torácico no cardiogénico, enfermedad por reflujo gastroesofágico, trastornos funcionales esofágicos, dolor torácico funcional, hipersensibilidad al reflujo, trastornos motores esofágicosResumen
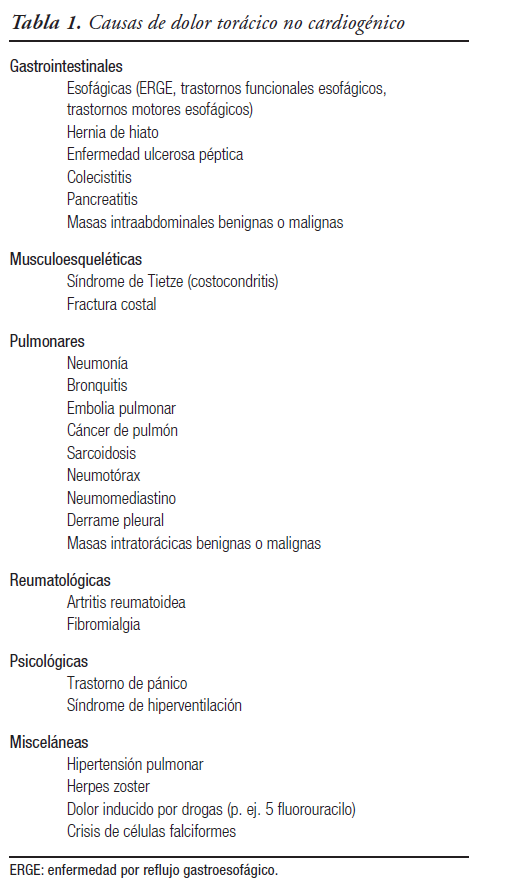
El dolor torácico no cardiogénico se define como la presencia de dolor retroesternal recurrente en el que la etiología cardiovascular ha sido descartada de manera objetiva. Se estima que su prevalencia global en la comunidad es del 13%. Nuestro enfoque en esta revisión se centrará en las causas esofágicas de dolor retroesternal, las cuales ocupan el primer lugar dentro de las causas no cardíacas. Las herramientas diagnósticas disponibles en la actualidad para evaluar los trastornos esofágicos relacionados con dolor torácico no cardiogénico incluyen: ensayos terapéuticos con inhibidores de bomba de protones, videoendoscopía digestiva alta, monitoreo ambulatorio de reflujo y manometría esofágica de alta resolución. El tratamiento debe estar dirigido al mecanismo fisiopatológico subyacente responsable de los síntomas. Las opciones terapéuticas incluyen fármacos (inhibidores de bomba de protones y neuromoduladores), tratamiento endoscópico, cirugía y terapias psicológicas.
Citas
-1. Gómez-Escudero O, Coss-Adame E, Amieva-Balmori M, et al. Consenso mexicano sobre dolor torácico no cardiaco. Revista de Gastroenterología de México 2019;84:372-397.
-2. Fass R, Achem SR. Noncardiac chest pain: epidemiology, natural course and pathogenesis. J Neurogastroenterol Motil 2011;17:110-123.
-3. Committee Members W, Gulati M, Levy PD. AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart... Journal of the American, https://www.jacc.org/doi/abs/10.1016/j.jacc.2021.07.053 (2021)
-4. Manterola C, Barroso MS, Losada H, et al. Prevalence of esophageal disorders in patients with recurrent chest pain. Dis Esophagus 2004;17:285-291.
-5. Wong WM, Lam KF, Cheng C, et al. Population based study of noncardiac chest pain in southern Chinese: prevalence, psychosocial factors and health care utilization. World J Gastroenterol 2004;10:707-712.
-6. Eslick GD, Coulshed DS, Talley NJ. Review article: the burden of illness of non-cardiac chest pain. Aliment Pharmacol Ther 2002;16:1217-1223.
-7. Ford AC, Suares NC, Talley NJ. Meta-analysis: the epidemiology of noncardiac chest pain in the community. Aliment Pharmacol Ther 2011;34:172-180.
-8. Chiocca JC, Olmos JA, Salis GB, et al. Prevalence, clinical spectrum and atypical symptoms of gastro-oesophageal reflux in Argentina: a nationwide population-based study. Aliment Pharmacol Ther 2005;22:331-342.
-9. Eslick GD, Jones MP, Talley NJ. Non-cardiac chest pain: prevalence, risk factors, impact and consulting-a population-based study. Aliment Pharmacol Ther 2003;17:1115-1124.
-10. Al-Ani M, Winchester DE. Prevalence and Overlap of Noncardiac Conditions in the Evaluation of Low-risk Acute Chest Pain Patients. Crit Pathw Cardiol 2015;14:97-102.
-11. Fass R, Fennerty MB, Johnson C, et al. Correlation of ambulatory 24-hour esophageal pH monitoring results with symptom improvement in patients with noncardiac chest pain (NCCP) due to gastroesophageal reflux disease (GERD). Gastroenterology 1998;114:A751.
-12. Dickman R, Emmons S, Cui H, et al. The effect of a therapeutic trial of high-dose rabeprazole on symptom response of patients with non-cardiac chest pain: a randomized, double-blind, placebo-controlled, crossover trial. Alimentary Pharmacology and Therapeutics 2005;22:547-555.
-13. Aziz Q, Fass R, Prakash Gyawali C, et al. Esophageal Disorders. Gastroenterology 2016;150:1368-1379.
-14. Fass R, Dickman R. Non-cardiac chest pain: an update. Neurogastroenterology and Motility 2006;18:408-417.
-15. Dellon ES, Liacouras CA, Molina-Infante J, et al. Updated International Consensus Diagnostic Criteria for Eosinophilic Esophagitis: Proceedings of the AGREE Conference. Gastroenterology 2018;155:1022-1033.e10.
-16. Achem SR, Almansa C, Krishna M, et al. Oesophageal eosinophilic infiltration in patients with noncardiac chest pain. Aliment Pharmacol Ther 2011;33:1194-1201.
-17. Gibbs JF, Rajput A, Chadha KS, et al. The changing profile of esophageal cancer presentation and its implication for diagnosis. J Natl Med Assoc 2007;99:620-626.
-18. Sengupta JN. Esophageal sensory physiology. GI Motility online. Epub ahead of print 16 May 2006. DOI: 10.1038/gimo16
-19. Richter JE, Bradley LA, Castell DO. Esophageal chest pain: current controversies in pathogenesis, diagnosis, and therapy. Ann Intern Med 1989;110:66-78.
-20. Paterson WG, Abdollah H, Beck IT, et al. Ambulatory esophageal manometry, pH-metry, and Holter ECG monitoring in patients with atypical chest pain. Dig Dis Sci 1993;38:795-802.
-21. Richter JE, Dalton CB, Bradley LA, et al. Oral nifedipine in the treatment of noncardiac chest pain in patients with the nutcracker esophagus. Gastroenterology 1987;93:21-28.
-22. Cannon RO 3rd, Benjamin SB. Chest pain as a consequence of abnormal visceral nociception. Dig Dis Sci 1993;38:193-196.
-23. Barish CF, Castell DO, Richter JE. Graded esophageal balloon distention. Dig Dis Sci 1986;31:1292-1298.
-24. Richter JE, Barish CF, Castell DO. Abnormal sensory perception in patients with esophageal chest pain. Gastroenterology 1986;91:845-852.
-25. Deschner WK, Maher KA, Cattau EL Jr, et al. Intraesophageal balloon distention versus drug provocation in the evaluation of noncardiac chest pain. Am J Gastroenterol 1990;85:938-943.
-26. Rao SS, Gregersen H, Hayek B, et al. Unexplained chest pain: the hypersensitive, hyperreactive, and poorly compliant esophagus. Annals of internal medicine 1996;124:950-958.
-27. Balaban DH, Yamamoto Y, Liu J, et al. Sustained esophageal contraction: a marker of esophageal chest pain identified by intraluminal ultrasonography. Gastroenterology 1999;116:29-37.
-28. Pehlivanov N, Liu J, Mittal RK. Sustained esophageal contraction: a motor correlate of heartburn symptom. Am J Physiol Gastrointest Liver Physiol 2001;281:G743-51.
-29. Mackenzie J, Land D, Belch J, et al. OESOPHAGEAL ISCHAEMIA IN MOTILITY DISORDERS ASSOCIATED WITH CHEST PAIN. Lancet 1988;332:592-595.
-30. McIntosh K, Paterson WG. Sustained esophageal longitudinal smooth muscle contraction may not be a cause of noncardiac chest pain. Neurogastroenterol Motil 2018;30:e13428.
-31. Yamasaki T, Fass R. Noncardiac chest pain: diagnosis and management. Curr Opin Gastroenterol 2017;33:293-300.
-32. Eslick GD, Coulshed DS, Talley NJ. Diagnosis and treatment of noncardiac chest pain. Nat Clin Pract Gastroenterol Hepatol 2005; 2:463-472.
-33. Fass R, Achem SR. Noncardiac chest pain: diagnostic evaluation. Dis Esophagus 2012;25:89-101.
-34. Fenster PE. Evaluation of chest pain: a cardiology perspective for gastroenterologists. Gastroenterol Clin North Am 2004;33:35-40.
-35. Pandak WM, Arezo S, Everett S, et al. Short course of omeprazole: a better first diagnostic approach to noncardiac chest pain than endoscopy, manometry, or 24-hour esophageal pH monitoring. J Clin Gastroenterol 2002;35:307-314.
-36. Achem SR, Kolts BE, Wears R, et al. Chest pain associated with nutcracker esophagus: a preliminary study of the role of gastroesophageal reflux. Am J Gastroenterol 1993;88:187-192.
-37. Achem SR, Kolts BE, MacMath T, et al. Effects of omeprazole versus placebo in treatment of noncardiac chest pain and gastroesophageal reflux. Dig Dis Sci 1997;42:2138-2145.
-38. Gasiorowska A, Fass R. The proton pump inhibitor (PPI) test in GERD: does it still have a role? J Clin Gastroenterol 2008;42:867-874.
-39. Schindlbeck NE, Klauser AG, Voderholzer WA, et al. Empiric therapy for gastroesophageal reflux disease. Arch Intern Med 1995;155:1808-1812.
-40. Fass R, Fennerty MB, Ofman JJ, et al. The clinical and economic value of a short course of omeprazole in patients with noncardiac chest pain. Gastroenterology 1998;115:42-49.
-41. Johnsson F, Weywadt L, Solhaug J-H, et al. One-week omeprazole treatment in the diagnosis of gastro-oesophageal reflux disease. Scand J Gastroenterol 1998;33:15-20.
-42. Fass R, Ofman JJ, Gralnek IM, et al. Clinical and economic assessment of the omeprazole test in patients with symptoms suggestive of gastroesophageal reflux disease. Arch Intern Med 1999;159:2161-2168.
-43. Bate CM, Riley SA, Chapman RW, et al. Evaluation of omeprazole as a cost-effective diagnostic test for gastro-oesophageal reflux disease. Aliment Pharmacol Ther 1999;13:59-66.
-44. Fass R, Ofman JJ, Sampliner RE, et al. The omeprazole test is as sensitive as 24-h oesophageal pH monitoring in diagnosing gastro-oesophageal reflux disease in symptomatic patients with erosive oesophagitis. Aliment Pharmacol Ther 2000;14:389-396.
-45. Fass R. Empirical trials in treatment of gastroesophageal reflux disease. Dig Dis 2000;18:20-26.
-46. Juul-Hansen P, Rydning A, Jacobsen CD, et al. High-dose proton-pump inhibitors as a diagnostic test of gastro-oesophageal reflux disease in endoscopic-negative patients. Scand J Gastroenterol 2001;36:806-810.
-47. Xia HHX, Lai KC, Lam SK, et al. Symptomatic response to lansoprazole predicts abnormal acid reflux in endoscopy-negative patients with non-cardiac chest pain. Aliment Pharmacol Ther 2003;17:369-377.
-48. Husser D, Bollmann A, Kühne C, et al. Evaluation of noncardiac chest pain: diagnostic approach, coping strategies and quality of life. Eur J Pain 2006;10:51-55.
-49. Kim JH, Sinn DH, Son HJ, et al. Comparison of one-week and two-week empirical trial with a high-dose rabeprazole in non-cardiac chest pain patients. Journal of Gastroenterology and Hepatology 2009;24:1504-1509.
-50. Flook NW, Moayyedi P, Dent J, et al. Acid-Suppressive Therapy With Esomeprazole for Relief of Unexplained Chest Pain in Primary Care: A Randomized, Double-Blind, Placebo-Controlled Trial. American Journal of Gastroenterology 2013;108:56-64.
-51. Cremonini F, Wise J, Moayyedi P, et al. Diagnostic and Therapeutic Use of Proton Pump Inhibitors in Non-Cardiac Chest Pain: A Metaanalysis. The American Journal of Gastroenterology 2005;100:1226-1232.
-52. Wang WH, Huang JQ, Zheng GF, et al. Is Proton Pump Inhibitor Testing an Effective Approach to Diagnose Gastroesophageal Reflux Disease in Patients With Noncardiac Chest Pain? Archives of Internal Medicine 2005;165:1222.
-53. Wertli MM, Ruchti KB, Steurer J, et al. Diagnostic indicators of non-cardiovascular chest pain: a systematic review and meta-analysis. BMC Medicine; 11. Epub ahead of print 2013. DOI: 10.1186/1741-7015-11-239
-54. Ghoneim S, El Hage Chehade N, Wang J, et al. S412 Diagnostic Accuracy of the Proton Pump Inhibitor Test in Patients With Gastroesophageal Reflux Disease and Non-Cardiac Chest Pain: A Systematic Review and Meta-Analysis. American Journal of Gastroenterology 2021;116:S182-S183.
-55. Yadlapati R, Prakash Gyawali C, Pandolfino JE, et al. AGA Clinical Practice Update on the Personalized Approach to the Evaluation and Management of GERD: Expert Review. Clinical Gastroenterology and Hepatology 2022;20:984-994.e1.
-56. Vela MF. Diagnostic Work-Up of GERD. Gastrointestinal Endoscopy Clinics of North America 2014;24:655-666.
-57. Sharma VK. Role of endoscopy in GERD. Gastroenterol Clin North Am 2014;43:39-46.
-58. ASGE Standards of Practice Committee, Muthusamy VR, Lightdale JR, et al. The role of endoscopy in the management of GERD. Gastrointest Endosc 2015;81:1305-1310.
-59. Hsia PC, Maher KA, Lewis JH, et al. Utility of upper endoscopy in the evaluation of noncardiac chest pain. Gastrointest Endosc 1991;37:22-26.
-60. Frøbert O, Funch-Jensen P, Jacobsen NO, et al. Upper endoscopy in patients with angina and normal coronary angiograms. Endoscopy 1995;27:365-370.
-61. García-Compeán D, González M, Galindo G, et al. Prevalence of gastroesophageal reflux disease in patients with extraesophageal symptoms referred from otolaryngology, allergy, and cardiology practices: a … Digestive, https://www.karger.com/Article/Abstract/51392 (2000).
-62. Wong W-M, Lai KC, Lau CP, et al. Upper gastrointestinal evaluation of Chinese patients with non-cardiac chest pain. Aliment Pharmacol Ther 2002;16:465-471.
-63. Battaglia E, Bassotti G, Buonafede G, et al. Noncardiac chest pain of esophageal origin in patients with and without coronary artery disease. Hepatogastroenterology 2005;52:792-795.
-64. Dickman R, Mattek N, Holub J, et al. Prevalence of upper gastrointestinal tract findings in patients with noncardiac chest pain versus those with gastroesophageal reflux disease (GERD)-related symptoms: results from a national endoscopic database. Am J Gastroenterol 2007;102:1173-1179.
-65. Williams JF, Sontag SJ, Schnell T, et al. Non-cardiac chest pain: the long-term natural history and comparison with gastroesophageal reflux disease. Am J Gastroenterol 2009;104:2145-2152.
-66. Katz PO, Dunbar KB, Schnoll-Sussman FH, et al. ACG Clinical Guideline for the Diagnosis and Management of Gastroesophageal Reflux Disease. Am J Gastroenterol 2022;117:27-56.
-67. Gyawali CP, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut 2018;67:1351-1362.
-68. Kim HP, Vance RB, Shaheen NJ, et al. The prevalence and diagnostic utility of endoscopic features of eosinophilic esophagitis: a meta-analysis. Clin Gastroenterol Hepatol 2012;10:988-96.e5.
-69. Dunbar KB, Agoston AT, Odze RD, et al. Association of Acute Gastroesophageal Reflux Disease With Esophageal Histologic Changes. JAMA 2016;315:2104-2112.
-70. Odiase E, Schwartz A, Souza RF, et al. New Eosinophilic Esophagitis Concepts Call for Change in Proton Pump Inhibitor Management Before Diagnostic Endoscopy. Gastroenterology 2018;154:1217-1221.e3.
-71. Pandolfino JE, Kahrilas PJ. Prolonged pH monitoring: Bravo capsule. Gastrointest Endosc Clin N Am 2005;15:307-318.
-72. Roman S, Gyawali CP, Savarino E, et al. Ambulatory reflux monitoring for diagnosis of gastro-esophageal reflux disease: Update of the Porto consensus and recommendations from an international consensus group. Neurogastroenterol Motil 2017;29:e13067.
-73. Lacima G, Grande L, Pera M, et al. Utility of ambulatory 24-hour esophageal pH and motility monitoring in noncardiac chest pain: report of 90 patients and review of the literature. Dig Dis Sci 2003;48:952-961.
-74. Streets CG, DeMeester TR. Ambulatory 24-hour esophageal pH monitoring: why, when, and what to do. J Clin Gastroenterol 2003;37:14-22.
-75. Demeester TR, O'sullivan GC, Bermudez G, et al. Esophageal Function in Patients with Angina-Type Chest Pain and Normal Coronary Angiograms. Annals of Surgery 1982;196:488-498.
-76. de Caestecker JS, Blackwell JN, Brown J, et al. The oesophagus as a cause of recurrent chest pain: which patients should be investigated and which tests should be used? Lancet 1985;2:1143-1146.
-77. Janssens J, Vantrappen G, Ghillebert G. 24-hour recording of esophageal pressure and pH in patients with noncardiac chest pain. Gastroenterology 1986;90:1978-1984.
-78. Schofield PM, Bennett DH, Whorwell PJ, et al. Exertional gastro-oesophageal reflux: a mechanism for symptoms in patients with angina pectoris and normal coronary angiograms. Br Med J 1987;294:1459-1461.
-79. Hewson EG, Dalton CB, Richter JE. Comparison of esophageal manometry, provocative testing, and ambulatory monitoring in patients with unexplained chest pain. Dig Dis Sci 1990;35:302-309.
-80. Hewson EG, Sinclair JW, Dalton CB, et al. Twenty-four-hour esophageal pH monitoring: the most useful test for evaluating noncardiac chest pain. Am J Med 1991;90:576-583.
-81. Prakash C, Clouse RE. Wireless pH monitoring in patients with non-cardiac chest pain. Am J Gastroenterol 2006;101:446-452.
-82. Prakash C, Jonnalagadda S, Azar R, et al. Endoscopic removal of the wireless pH monitoring capsule in patients with severe discomfort. Gastrointest Endosc 2006;64:828-832.
-83. Herregods TVK, Bredenoord AJ, Oors JM, et al. Determinants of the Association between Non-Cardiac Chest Pain and Reflux. Am J Gastroenterol 2017;112:1671-1677.
-84. Ribolsi M, Balestrieri P, Biasutto D, et al. Role of Mixed Reflux and Hypomotility with Delayed Reflux Clearance in Patients with Non-cardiac Chest Pain. J Neurogastroenterol Motil 2016;22:606-612.
-85. Min YW, Choi K, Pyo JH, et al. Impaired Esophageal Mucosal Integrity May Play a Causative Role in Patients With Nongastroesophageal Reflux Disease-Related Noncardiac Chest Pain. Medicine 2015;94:e2295.
-86. Katz PO, Dalton CB, Richter JE, et al. Esophageal testing of patients with noncardiac chest pain or dysphagia. Results of three years’ experience with 1161 patients. Ann Intern Med 1987;106:593-597.
-87. Dekel R, Pearson T, Wendel C, et al. Assessment of oesophageal motor function in patients with dysphagia or chest pain - the Clinical Outcomes Research Initiative experience. Alimentary Pharmacology & Therapeutics 2003;18:1083-1089.
-88. Akinsiku O, Yamasaki T, Brunner S, et al. High resolution vs conventional esophageal manometry in the assessment of esophageal motor disorders in patients with non-cardiac chest pain. Neurogastroenterol Motil 2018;30:e13282.
-89. Lemme EM, Moraes-Filho JP, Domingues G, et al. Manometric findings of esophageal motor disorders in 240 Brazilian patients with non-cardiac chest pain. Dis Esophagus 2000;13:117-121.
-90. Yadlapati R, Kahrilas PJ, Fox MR, et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0©. Neurogastroenterol Motil 2021;33:e14058.
-91. Gomez Cifuentes J, Lopez R, Thota PN. Factors predictive of gastroesophageal reflux disease and esophageal motility disorders in patients with non-cardiac chest pain. Scand J Gastroenterol 2018;53:643-649.
-92. Johnston BT, Troshinsky MB, Castell JA, et al. Comparison of barium radiology with esophageal pH monitoring in the diagnosis of gastroesophageal reflux disease. Am J Gastroenterol 1996;91:1181-1185.
-93. Roman S, Kahrilas PJ. Distal Esophageal Spasm. Dysphagia 2012;27:115-123.
-94. Schima W, Stacher G, Pokieser P, et al. Esophageal motor disorders: videofluoroscopic and manometric evaluation-prospective study in 88 symptomatic patients. Radiology 1992;185:487-491.
-95. Neyaz Z, Gupta M, Ghoshal UC. How to Perform and Interpret Timed Barium Esophagogram. Journal of Neurogastroenterology and Motility 2013;19:251-256.
-96. Min YW, Rhee P-L. Esophageal hypersensitivity in noncardiac chest pain. Ann N Y Acad Sci 2016;1380:27-32.
-97. Bernstein LM, Baker LA. A Clinical Test For Esophagitis. Gastroenterology 1958;34:760-781.
-98. Fass R, Naliboff B, Higa L, et al. Differential effect of long-term esophageal acid exposure on mechanosensitivity and chemosensitivity in humans. Gastroenterology 1998;115:1363-1373.
-99. Nasr I, Attaluri A, Coss-Adame E, et al. Diagnostic utility of the oesophageal balloon distension test in the evaluation of oesophageal chest pain. Alimentary Pharmacology & Therapeutics 2012;35:1474-1481.
-100. Nasr I, Attaluri A, Hashmi S, et al. Investigation of esophageal sensation and biomechanical properties in functional chest pain. Neurogastroenterology & Motility. Epub ahead of print 2010. DOI: 10.1111/j.1365-2982.2009.01451.x
-101. Drewes AM, Schipper K-P, Dimcevski G, et al. Multi-modal induction and assessment of allodynia and hyperalgesia in the human oesophagus. European Journal of Pain 2003;7:539-549.
-102. Clouse RE, Carney RM. The psychological profile of non-cardiac chest pain patients. Eur J Gastroenterol Hepatol 1995;7:1160-1165. -103. Campbell KA, Madva EN, Villegas AC, et al. Non-cardiac Chest Pain: A Review for the Consultation-Liaison Psychiatrist. Psychosomatics 2017;58:252-265.
-104. Ortiz-Olvera NX, González-Martínez M, Ruiz-Flores LG, et al. [Causes of non-cardiac chest pain: multidisciplinary perspective]. Rev Gastroenterol Mex 2007;72:92-99.
-105. Clouse RE, Lustman PJ. Psychiatric illness and contraction abnormalities of the esophagus. N Engl J Med 1983;309:1337-1342.
-106. Yamasaki T, Fass R. Noncardiac chest pain. Current Opinion in Gastroenterology 2017;33:293-300.
-107. Lima JJ, Franciosi JP. Pharmacogenomic testing: the case for CYP2C19 proton pump inhibitor gene-drug pairs. Pharmacogenomics 2014;15:1405-1416.
-108. Graham DY, Tansel A. Interchangeable Use of Proton Pump Inhibitors Based on Relative Potency. Clin Gastroenterol Hepatol 2018;16:800-808.e7.
-109. Bautista J, Fullerton H, Briseno M, et al. The effect of an empirical trial of high-dose lansoprazole on symptom response of patients with non-cardiac chest pain - a randomized, double-blind, placebo-controlled, crossover trial. Alimentary Pharmacology & Therapeutics 2004;19:1123-1130.
-110. Borjesson M, Rolny P, Mannheimer C, et al. Nutcracker oesophagus: a double-blind, placebo-controlled, cross-over study of the effects of lansoprazole. Alimentary Pharmacology & Therapeutics 2003;18:1129-1135.
-111. Burgstaller JM, Jenni BF, Steurer J, et al. Treatment Efficacy for Non-Cardiovascular Chest Pain: A Systematic Review and Meta-Analysis. PLoS ONE 2014;9:e104722.
-112. Abdul Kadir NP, Ma ZF, Abdul Hafidz MI, et al. Comparing Efficacy and Safety of Empirical vs. Guided Therapy for Non-cardiac Chest Pain: A Pragmatic Randomized Trial. Front Med 2021;8:605647.
-113. Konturek JW, Gillessen A, Domschke W. Diffuse Esophageal Spasm: A Malfunction That Involves Nitric Oxide? Scandinavian Journal of Gastroenterology 1995;30:1041-1045.
-114. Cattau EL Jr, Castell DO, Johnson DA, et al. Diltiazem therapy for symptoms associated with nutcracker esophagus. Am J Gastroenterol 1991;86:272-276.
-115. Fox M, Sweis R, Wong T, et al. Sildenafil relieves symptoms and normalizes motility in patients with oesophageal spasm: a report of two cases. Neurogastroenterol Motil 2007;19:798-803.
-116. Storr M, Allescher HD, Rösch T, et al. Treatment of symptomatic diffuse esophageal spasm by endoscopic injections of botulinum toxin: a prospective study with long-term follow-up. Gastrointest Endosc 2001;54:754-759.
-117. Miller LS, Pullela SV, Parkman HP, et al. Treatment of Chest Pain in Patients With Noncardiac, Nonreflux, Nonachalasia Spastic Esophageal Motor Disorders Using Botulinum Toxin Injection Into The Gastroesophageal Junction. American Journal of Gastroenterology 2002;97:1640-1646.
-118. Vanuytsel T, Bisschops R, Farré R, et al. Botulinum toxin reduces Dysphagia in patients with nonachalasia primary esophageal motility disorders. Clin Gastroenterol Hepatol 2013;11:1115-1121.e2.
-119. Winters C, Artnak EJ, Benjamin SB, et al. Esophageal bougienage in symptomatic patients with the nutcracker esophagus. A primary esophageal motility disorder. JAMA 1984;252:363-366.
-120. Irving JD, Owen WJ, Linsell J, et al. Management of diffuse esophageal spasm with balloon dilatation. Gastrointest Radiol 1992;17:189-192.
-121. Sharata AM, Dunst CM, Pescarus R, et al. Peroral endoscopic myotomy (POEM) for esophageal primary motility disorders: analysis of 100 consecutive patients. J Gastrointest Surg 2015;19:161-70; discussion 170.
-122. Andolfi C, Fisichella PM. Meta-analysis of clinical outcome after treatment for achalasia based on manometric subtypes. Br J Surg 2019;106:332-341.
-123. Khan MA, Kumbhari V, Ngamruengphong S, et al. Is POEM the Answer for Management of Spastic Esophageal Disorders? A Systematic Review and Meta-Analysis. Dig Dis Sci 2017;62:35-44.
-124. Khashab MA, Familiari P, Draganov PV, et al. Peroral endoscopic myotomy is effective and safe in non-achalasia esophageal motility disorders: an international multicenter study. Endosc Int Open 2018;6:E1031-E1036.
-125. Albers D, Frieling T, Dakkak D, et al. Peroral endoscopic myotomy (POEM) is effective in treatment of noncardiac chest pain caused by hypercontractile esophageal motility disorders: results of the POEM-HYPE-Study. Z Gastroenterol 2018;56:1337-1342.
-126. Leconte M, Douard R, Gaudric M, et al. Functional results after extended myotomy for diffuse oesophageal spasm. Br J Surg 2007;94:1113-1118.
-127. Zikos TA, Triadafilopoulos G, Clarke JO. Esophagogastric Junction Outflow Obstruction: Current Approach to Diagnosis and Management. Curr Gastroenterol Rep 2020;22:9.
-128. Clayton SB, Shin CM, Ewing A, et al. Pneumatic dilation improves esophageal emptying and symptoms in patients with idiopathic esophago-gastric junction outflow obstruction. Neurogastroenterol Motil 2019;31:e13522.
-129. Filicori F, Dunst CM, Sharata A, et al. Long-term outcomes following POEM for non-achalasia motility disorders of the esophagus. Surg Endosc 2019;33:1632-1639.
-130. Patel DA, Yadlapati R, Vaezi MF. Esophageal Motility Disorders: Current Approach to Diagnostics and Therapeutics. Gastroenterology 2022;162:1617-1634.
-131. Fass R, Shibli F, Tawil J. Diagnosis and Management of Functional Chest Pain in the Rome IV Era. Journal of Neurogastroenterology and Motility 2019;25:487-498.
-132. Drossman DA, Tack J, Ford AC, et al. Neuromodulators for Functional Gastrointestinal Disorders (Disorders of Gut−Brain Interaction): A Rome Foundation Working Team Report. Gastroenterology 2018;154:1140-1171.e1.
-133. Cannon RO, Quyyumi AA, Mincemoyer R, et al. Imipramine in Patients with Chest Pain Despite Normal Coronary Angiograms. New England Journal of Medicine 1994;330:1411-1417.
-134. Kaski JC, Cox ID, Robert Crook J, et al. Differential plasma endothelin levels in subgroups of patients with angina and angiographically normal coronary arteries. American Heart Journal 1998;136:412-417.
-135. Maradey-Romero C, Fass R. New therapies for non-cardiac chest pain. Curr Gastroenterol Rep 2014;16:390.
-136. Dickman R, Maradey-Romero C, Fass R. The role of pain modulators in esophageal disorders - no pain no gain. Neurogastroenterology & Motility 2014;26:603-610.
-137. Sindrup SH, Otto M, Finnerup NB, et al. Antidepressants in the treatment of neuropathic pain. Basic Clin Pharmacol Toxicol 2005;96:399-409.
-138. Atluri DK, Chandar AK, Fass R, et al. Systematic review with meta-analysis: selective serotonin reuptake inhibitors for noncardiac chest pain. Aliment Pharmacol Ther 2015;41:167-176.
-139. Doraiswamy PM, Varia I, Hellegers C, et al. A randomized controlled trial of paroxetine for noncardiac chest pain. Psychopharmacol Bull 2006;39:15-24.
-140. Spinhoven P, Van der Does AJW, Van Dijk E, et al. Heart-focused anxiety as a mediating variable in the treatment of noncardiac chest pain by cognitive-behavioral therapy and paroxetine. Journal of Psychosomatic Research 2010;69 227-235.
-141. Varia I, Logue E, O’Connor C, et al. Randomized trial of sertraline in patients with unexplained chest pain of noncardiac origin. American Heart Journal 2000;140:367-372.
-142. Keefe FJ, Shelby RA, Somers TJ, et al. Effects of coping skills training and sertraline in patients with non-cardiac chest pain: A randomized controlled study. Pain 2011;152:730-741.
-143. Gutierrez MA, Stimmel GL, Aiso JY. Venlafaxine: A 2003 update. Clinical Therapeutics 2003;25:2138-2154.
-144. Lee H, Kim JH, Min B-H, et al. Efficacy of Venlafaxine for Symptomatic Relief in Young Adult Patients With Functional Chest Pain: A Randomized, Double-Blind, Placebo-Controlled, Crossover Trial. American Journal of Gastroenterology 2010;105:1504-1512.
-145. Viazis N, Keyoglou A, Kanellopoulos AK, et al. Selective serotonin reuptake inhibitors for the treatment of hypersensitive esophagus: a randomized, double-blind, placebo-controlled study. Am J Gastroenterol 2012;107:1662-1667.
-146. Manolakis AC, Broers C, Geysen H, et al. Effect of citalopram on esophageal motility in healthy subjects-Implications for reflux episodes, dysphagia, and globus. Neurogastroenterol Motil 2019;31:e13632.
-147. Rao SSC, Mudipalli RS, Mujica V, et al. Digestive Diseases and Sciences. 2002;47:2763-2768.
-148. Rao SSC, Mudipalli RS, Remes-Troche JM, et al. Theophylline Improves Esophageal Chest Pain? A Randomized, Placebo-Controlled Study. The American Journal of Gastroenterology 2007;102:930-938.
-149. Jaggar SI, Hasnie FS, Sellaturay S, et al. The anti-hyperalgesic actions of the cannabinoid anandamide and the putative CB2 receptor agonist palmitoylethanolamide in visceral and somatic inflammatory pain. Pain 1998;76:189-199.
-150. Malik Z, Bayman L, Valestin J, et al. Dronabinol increases pain threshold in patients with functional chest pain: a pilot double-blind placebo-controlled trial. Dis Esophagus 2017;30:1-8.
-151. Keefer L, Palsson OS, Pandolfino JE. Best Practice Update: Incorporating Psychogastroenterology Into Management of Digestive Disorders. Gastroenterology 2018;154:1249-1257.
-152. Kisely SR, Campbell LA, Yelland MJ, et al. Psychological interventions for symptomatic management of non-specific chest pain in patients with normal coronary anatomy. Cochrane Database Syst Rev 2015;CD004101.
-153. Jonsbu E, Dammen T, Morken G, et al. Short-term cognitive behavioral therapy for non-cardiac chest pain and benign palpitations: a randomized controlled trial. J Psychosom Res 2011;70:117-123.
-154. Riehl ME, Keefer L. Hypnotherapy for Esophageal Disorders. American Journal of Clinical Hypnosis 2015;58:22-33.
-155. Vasant DH, Whorwell PJ. Gut-focused hypnotherapy for Functional Gastrointestinal Disorders: Evidence-base, practical aspects, and the Manchester Protocol. Neurogastroenterol Motil 2019;31:e13573.
-156. Riehl ME, Pandolfino JE, Palsson OS, et al. Feasibility and acceptability of esophageal-directed hypnotherapy for functional heartburn. Diseases of the Esophagus 2016;29:490-496.
-157. Jones H. Treatment of non-cardiac chest pain: a controlled trial of hypnotherapy. Gut 2006;55:1403-1408.
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2022 Mercedes Manresa, Paula Cecilia Carboné, Guillermina Diez

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.












