La enfermedad del hígado graso no alcohólico y el sexo masculino son factores de riesgo para el adenoma colorrectal: un análisis retrospectivo
DOI:
https://doi.org/10.52787/agl.v54i3.428Palabras clave:
Enfermedad del hígado graso no alcohólico, adenoma colorrectal, factor de riesgo, PerúResumen
Objective. Although the causes of colorectal adenoma have been well characterized in other populations, this study is the first to investigate the risk factors for colorectal adenoma in a Peruvian population.
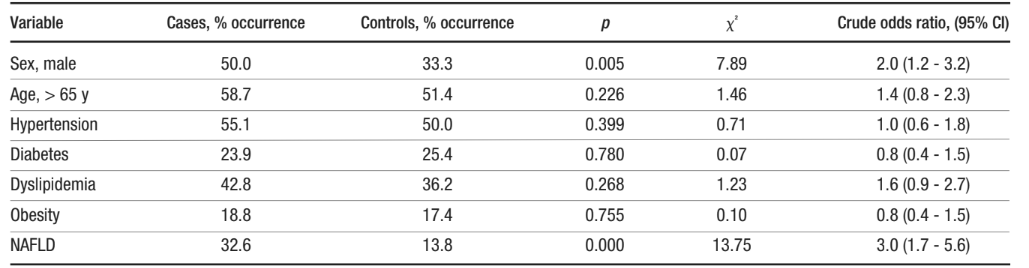
Material and Methods. This is an observational, retrospective, case-control study of patients who underwent colonoscopy at the gastroenterology service of a large hospital in northern Peru between 2015 and 2020. Two groups of 138 patients were selected based on colorectal adenoma diagnosis. Gender, age, and the presence of non-alcoholic fatty liver disease, diabetes, obesity, hypertension and dyslipidemia were compared between groups to calculate risk factors for colorectal adenoma. These are known risk factors in other populations.
Results. Among the measured factors, non-alcoholic fatty liver disease and male sex were found to be associated with colorectal adenoma (OR 3.3, >95% CI Interval 1.8-6.1 for non-alcoholic fatty liver disease, and OR 2.2 95% CI 1.3-3.6 for male sex). Other socio-medical characteristics did not reach statistical significance. Furthermore, no significant differences in location, number, size, endoscopic classification, histology or presence of advanced adenoma were observed when comparing patients diagnosed with non-alcoholic fatty liver disease with patients without this condition.
Conclusion. This study suggests that non-alcoholic fatty liver disease and male sex are positively associated with the diagnosis of colorectal adenoma in Peruvians. This indicates the need for more careful screening of these demographics.
Citas
-1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA: A Cancer Journal for Clinicians. 2021;71(3):209-49. Available from: https://doi.org/10.3322/caac.21660
-2. Nguyen LH, Goel A, Chung DC. Pathways of Colorectal Carcinogenesis. Gastroenterology. 2020 Jan;158(2):291-302. Available from: https://doi.org/10.1053/j.gastro.2019.08.059
-3. Galeș LN, Păun MA, Anghel RM, Trifă nescu OG. Cancer Screening: Present Recommendations, the Development of Multi-Cancer Early Development Tests, and the Prospect of Universal Cancer Screening. Cancers (Basel). 2024 Mar 18;16(6):1191. Available from: https://doi.org/10.3390/cancers16061191
-4. Areia M, Spaander MC, Kuipers EJ, Dinis-Ribeiro M. Endoscopic screening for gastric cancer: A cost-utility analysis for countries with an intermediate gastric cancer risk. United European Gastroenterol J. 2018 Mar;6(2):192-202. Available from: https://doi.org/10.1177/2050640617722902
-5. Steck SE, Guinter M, Zheng J, Thomson CA. Index-based dietary patterns and colorectal cancer risk: a systematic review. Adv Nutr. 2015 Nov;6(6):763-73. Available from: https://doi.org/10.3945/an.115.009746
-6. Giovannucci E. Modifiable risk factors for colon cancer. Gastroenterol Clin North Am. 2002 Dec;31(4):925-43. Available from: https://doi.org/10.1016/s0889-8553(02)00057-2
-7. Jasperson KW, Tuohy TM, Neklason DW, Burt RW. Hereditary and familial colon cancer. Gastroenterology. 2010 Jun;138(6):2044-58. Available from: https://doi.org/10.1053/j.gastro.2010.01.054
-8. O’Sullivan DE, Sutherland RL, Town S, Chow K, Fan J, Forbes N, et al. Risk Factors for Early-Onset Colorectal Cancer: A Systematic Review and Meta-analysis. Clinical Gastroenterology and Hepatology. 2022 Jun 1;20(6):1229-1240.e5. Available from: https://doi.org/10.1016/j.cgh.2021.01.037
-9. Sninsky JA, Shore BM, Lupu GV, Crockett SD. Risk Factors for Colorectal Polyps and Cancer. GastrointestEndosc Clin N Am. 2022 Apr;32(2):195-213. Available from: https://doi.org/10.1016/j.giec.2021.12.008
-10. Sun L, Yu S. Diabetes Mellitus Is an Independent Risk Factor for Colorectal Cancer. Dig Dis Sci. 2012 Jun 1;57(6):1586-97. Available from: https://doi.org/10.1007/s10620-012-2059-x
-11. Shen X, Wang Y, Zhao R, Wan Q, Wu Y, Zhao L, et al. Metabolic syndrome and the risk of colorectal cancer: a systematic review and meta-analysis. Int J Colorectal Dis. 2021 Oct 1;36(10):2215-25. Available from: https://doi.org/10.1007/s00384-021-03974-y
-12. Liu SS, Ma XF, Zhao J, Du SX, Zhang J, Dong MZ, et al. Association between nonalcoholic fatty liver disease and extrahepatic cancers: a systematic review and meta-analysis. Lipids in Health and Disease [Internet]. 2020 May 31 [cited 2024 May 30];19(1):118. Available from: https://doi.org/10.1186/s12944020-01288-6
-13. Grahn SW, Varma MG. Factors that Increase Risk of Colon Polyps. Clin Colon Rectal Surg [Internet]. 2008 Nov;21(4):247-55. Available from: https://doi.org/10.1055/s-0028-1089939
-14. Menon G, Recio-Boiles A, Lotfollahzadeh S, Cagir B. Colon Cancer. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 [cited 2024 May 31]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK470380/
-15. He X, Wu K, Ogino S, Giovannucci EL, Chan AT, Song M. Association Between Risk Factors for Colorectal Cancer and Risk of Serrated Polyps and Conventional Adenomas. Gastroenterology. 2018 Aug;155(2):355-373.e18. Available from: https://doi.org/10.1053/j.gastro.2019.06.039
-16. Wu H, Zhang J, Zhou B. Metabolic syndrome and colorectal adenoma risk: A systematic review and meta‑analysis. Clin Res Hepatol Gastroenterol. 2021 Sep;45(5):101749. Available from: https://doi.org/10.1016/j.clinre.2021.101749
-17. Okabayashi K, Ashrafian H, Hasegawa H, Yoo JH, Patel VM, Harling L, et al. Body Mass Index Category as a Risk Factor for Colorectal Adenomas: A Systematic Review and Meta-Analysis. Official journal of the American College of Gastroenterology | ACG. 2012 Aug;107(8):1175. Available from: https://doi.org/10.1038/ajg.2012.180
-18. Tian Y, Wang K, Li J, Wang J, Wang Z, Fan Y, et al. The association between serum lipids and colorectal neoplasm: a systemic review and meta-analysis. Public Health Nutrition. 2015 Dec;18(18):3355-70. Available from: https://doi.org/10.1017/s1368980015000646
-19. Godos J, Bella F, Torrisi A, Sciacca S, Galvano F, Grosso G. Dietary patterns and risk of colorectal adenoma: a systematic review and meta-analysis of observational studies. J Hum Nutr Diet. 2016 Dec;29(6):757-67. Available from: https://doi.org/10.1111/jhn.12395
-20. Manikat R, Nguyen MH. Nonalcoholic fatty liver disease and non-liver comorbidities. Clin Mol Hepatol. 2023 Jan 5;29(Suppl):s86-102. Available from: https://doi.org/10.3350/cmh.2022.0442
-21. Parizadeh SM, Parizadeh SA, Alizade-Noghani M, Jafarzadeh-Esfehani R, Ghandehari M, Mottaghi-Moghaddam A, et al. Association between non-alcoholic fatty liver disease and colorectal cancer. Expert Review of Gastroenterology & Hepatology. 2019 Jul 3;13(7):633-41. Available from: https://doi.org/10.1080/17474124.2019.1617696
-22. Wu PH, Chung CH, Wang YH, Hu JM, Chien WC, Cheng YC. Association between nonalcoholic fatty liver disease and colorectal cancer: A population-based study. Medicine. 2023 May 26;102(21):e33867. Available from: https://doi.org/10.1097/md.0000000000033867
-23. Huang KW, Leu HB, Wang YJ, Luo JC, Lin HC, Lee FY, et al. Patients with nonalcoholic fatty liver disease have higher risk of colorectal adenoma after negative baseline colonoscopy. Colorectal Disease. 2013;15(7):830-5. Available from: https://doi.org/10.1111/codi.12172
-24. Blackett JW, Verna EC, Lebwohl B. Increased Prevalence of Colorectal Adenomas in Patients with Nonalcoholic Fatty Liver Disease: A Cross-Sectional Study. Dig Dis. 2020;38(3):222-30. Available from: https://doi.org/10.1159/000502684
-25. Chen J, Bian D, Zang S, Yang Z, Tian G, Luo Y, et al. The association between nonalcoholic fatty liver disease and risk of colorectal adenoma and cancer incident and recurrence: a meta-analysis of observational studies. Expert Review of Gastroenterology & Hepatology. 2019 Apr 3;13(4):385-95. Available from: https://doi.org/10.1080/17474124.2019.1580143
-26. Li Y, Liu S, Gao Y, Ma H, Zhan S, Yang Y, et al. Association between NAFLD and Risk of Colorectal Adenoma in Chinese Han Population. Journal of Clinical and Translational Hepatology. 2019 Jun 28;7(2):99-105. Available from: https://doi.org/10.14218/jcth.2019.00010
-27. Liu M, Dai F, Peng Q. Relationship between severity of liver fibrosis and colorectal adenomatous polyp in nonalcoholic fatty liver disease. Chin J IntegrTradit West Med Dig. 2022 Jan 15;30(1):36-41. Available from: https://zxyxhen.whuhzzs.com/article/doi/10.3969/j.issn.1671-038X.2022.01.08
-28. Chuan LX, Chang J, Zhao JH, Li LH, Yang XY, Yu D. Association between nonalcoholic fatty liver disease and colorectal adenomatous polyps. J Clin Hepatol. 2020 Jun 20;36(6):1299-303. Available from: https://www.lcgdbzz.org/en/article/doi/10.3969/j.issn.1001-5256.2020.06.022
-29. Ye S, Liu Y, Zhang T, Feng H, Liu Y, Ma L. Analysis of the correlation between non-alcoholic fatty liver disease and the risk of colorectal neoplasms. Front Pharmacol. 2022 Nov 9;13. Available from: https://doi.org/10.3389/fphar.2022.1068432
-30. Lee JM, Park YM, Yun JS, Ahn YB, Lee KM, Kim DB, et al. The association between nonalcoholic fatty liver disease and esophageal, stomach, or colorectal cancer: National population-based cohort study. PLOS ONE. 2020 Jan 24;15(1):e0226351. Available from: https://doi.org/10.1371/journal.pone.0226351
-31. Chen W, Wang M, Jing X, Wu C, Zeng Y, Peng J, et al. High risk of colorectal polyps in men with non-alcoholic fatty liver disease: A systematic review and meta-analysis. Journal of Gastroenterology and Hepatology. 2020;35(12):2051-65. Available from: https://doi.org/10.1111/jgh.15158
-32. Pan S, Hong W, Wu W, Chen Q, Zhao Q, Wu J, et al. The relationship of nonalcoholic fatty liver disease and metabolic syndrome for colonoscopy colorectal neoplasm. Medicine. 2017 Jan;96(2):e5809. Available from: https://doi.org/10.1097/md.0000000000005809
-33. Chen QF, Zhou XD, Sun YJ, Fang DH, Zhao Q, Huang JH, et al. Sex-influenced association of non-alcoholic fatty liver disease with colorectal adenomatous and hyperplastic polyps. World Journal of Gastroenterology. 2017 Jul 28;23(28):5206-15. Available from: https://doi.org/10.3748/wjg.v23.i28.5206
-34. Ding W, Fan J, Qin J. Association between nonalcoholic fatty liver disease and colorectal adenoma: a systematic review and meta-analysis. Int J Clin Exp Med. 2015;8(1):322-33. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4358458/
-35. Lin X, You F, Liu H, Fang Y, Jin S, Wang Q. Site-specific risk of colorectal neoplasms in patients with non-alcoholic fatty liver disease: A systematic review and meta-analysis. PLOS ONE. 2021 Jan 25;16(1):e0245921. Available from: https://doi.org/10.1371/journal.pone.0245921
-36. Mitsala A, Tsalikidis C, Romanidis K, Pitiakoudis M. Non-Alcoholic Fatty Liver Disease and Extrahepatic Cancers: A Wolf in Sheep’s Clothing? Curr Oncol. 2022 Jun 25;29(7):4478-510. Available from: https://doi.org/10.3390/curroncol29070356
-37. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016 Jul;64(1):73-84. Available from: https://doi.org/10.1002/hep.28431
-38. Marjot T, Moolla A, Cobbold JF, Hodson L, Tomlinson JW. Nonalcoholic Fatty Liver Disease in Adults: Current Concepts in Etiology, Outcomes, and Management. Endocrine Reviews. 2020 Feb 1;41(1):66-117. Available from: https://doi.org/10.1210/endrev/bnz009
-39. Pouwels S, Sakran N, Graham Y, Leal A, Pintar T, Yang W, et al. Non-alcoholic fatty liver disease (NAFLD): a review of pathophysiology, clinical management and effects of weight loss. BMC EndocrDisord. 2022 Mar 14;22:63. Available from: https://doi.org/10.1186/s12902-022-00980-1
-40. Risk Factor Collaboration. NCD-RisC [Internet]. [cited 2024 May 26]. Available from: https://ncdrisc.org/data-downloads-adiposity.html
-41. Lai EJ, Calderwood AH, Doros G, Fix OK, Jacobson BC. The Boston bowel preparation scale: a valid and reliable instrument for colonoscopy-oriented research. GastrointestEndosc. 2009 Mar;69(3 Pt 2):620-5. Available from: https://doi.org/10.1016/j.gie.2008.05.057
-42. Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension [Internet]. 2020 Jun [cited 2024 May 29];75(6):1334-57. Available from: https://www.doi.org/10.1161/HYPERTENSIONAHA.120.15026
-43. ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes-2023. Diabetes Care [Internet]. 2022 Dec 12 [cited 2024 May 29];46(Supplement_1):S19-40. Available from: https://doi.org/10.2337/dc23-S002
-44. Pappan N, Awosika AO, Rehman A. Dyslipidemia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 [cited 2024 May 29]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK560891/
-45. Apovian CM. Obesity: definition, comorbidities, causes, and burden. Am J Manag Care. 2016 Jun;22(7 Suppl):s176-185. Available from: https://www.ajmc.com/view/obesity-definition-comorbidities-causes-burden
-46. Wong VWS, Wong GLH, Tsang SWC, Fan T, Chu WCW, Woo J, et al. High prevalence of colorectal neoplasm in patients with non-alcoholic steatohepatitis. Gut. 2011 Jun;60(6):829-36. Available from: https://doi.org/10.1136/gut.2011.237974
-47. Hwang ST, Cho YK, Park JH, Kim HJ, Park DI, Sohn CI, et al. Relationship of non-alcoholic fatty liver disease to colorectal adenomatous polyps. Journal of Gastroenterology and Hepatology. 2010;25(3):562-7. Available from: https://doi.org/10.1111/j.1440-1746.2009.06117.x
-48. Choi Y, Kim N. Sex Difference of Colon Adenoma Pathway and Colorectal Carcinogenesis. World J Mens Health. 2024 Apr;42(2):256-82. Available from: https://doi.org/10.5534%2Fwjmh.230085
-49. Shen H, Lipka S, Kumar A, Mustacchia P. Association between nonalcoholic fatty liver disease and colorectal adenoma: a systemic review and meta-analysis. Journal of Gastrointestinal Oncology. 2014 Dec;5(6). Available from: https://doi.org/10.3978%2Fj.issn.2078-6891.2014.061
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2024 Víctor Hugo Bardales-Zuta, Sandra Reyes-Aroca, Miguel de los Santos Verona-Escurra, Heber Giancarlo Moya-Carranza, Lissett Jeanette Fernández - Rodríguez

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.












