Los procedimientos quirúrgicos para la enfermedad por reflujo gastroesofágico
DOI:
https://doi.org/10.52787/agl.v55i4.553Palabras clave:
Enfermedad por reflujo gastroesofágico, cirugía antirreflujo, funduplicatura, hernia hiatal, cirugía laparoscópica, cirugía robóticaResumen
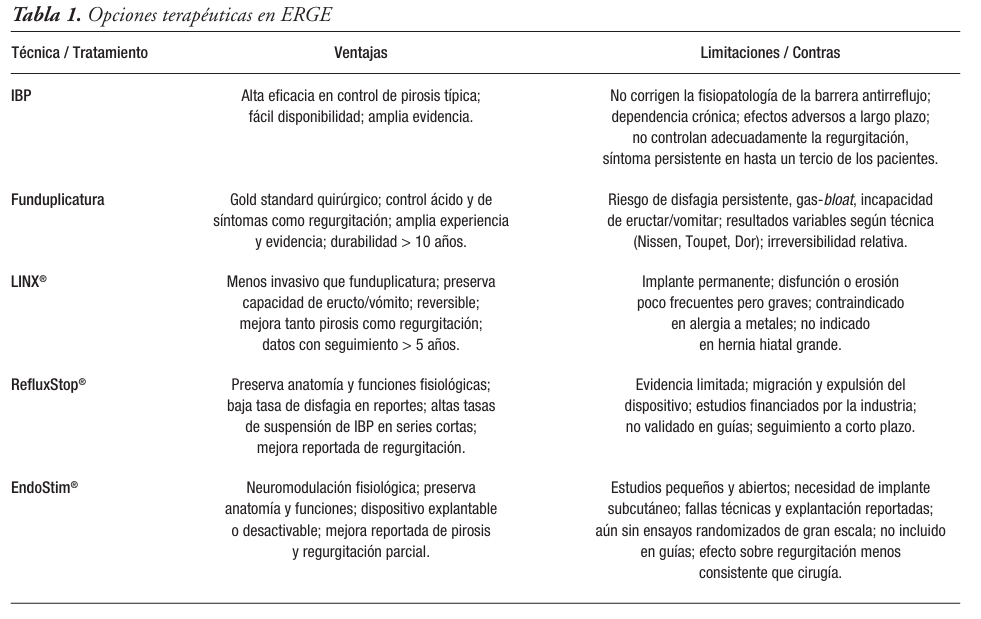
La enfermedad por reflujo gastroesofágico representa una condición prevalente a nivel mundial con impacto significativo en la calidad de vida de los pacientes y una carga creciente para los sistemas de salud. En Argentina, se estima una prevalencia del 23% de síntomas típicos semanales, similar a lo reportado en otras regiones de Latinoamérica. Aunque la mayoría de los pacientes con esofagitis responden adecuadamente a los inhibidores de la bomba de protones, hasta un 30 a 40% de los casos puede mostrar una respuesta parcial o inadecuada, especialmente en aquellos con enfermedad no erosiva. En tal contexto, la cirugía es una alternativa válida y efectiva. Esta revisión tiene como objetivo analizar de manera actualizada y basada en evidencia la evaluación funcional preoperatoria, las técnicas quirúrgicas, la selección de los pacientes y la relación entre la enfermedad por reflujo gastroesofágico y condiciones especiales como obesidad o enfermedades reumatológicas.
Citas
-1. Olmos JA, Pandolfino JE, Piskorz MM, et al. Latin American consensus on diagnosis of gastroesophageal reflux disease. Neurogastroenterol Motil. 2024;36(3):e14735. DOI:10.1111/nmo.14735
-2. Eusebi LH, Ratnakumaran R, Yuan Y, Solaymani-Dodaran M, Bazzoli F, Ford AC. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: A meta-analysis. Gut. 2018;67(3):430-40.
-3. El-Serag HB, Sweet S, Winchester CC, Dent J. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2014;63(6):871-880.
-4. Tack J, Pandolfino JE. Pathophysiology of gastroesophageal reflux disease: new understanding in a new era. Neurogastroenterol Motil. 2018;30(1):e13246.
-5. Gyawali CP, Yadlapati R, Fass R, et al. Updates to the modern diagnosis of GERD: Lyon consensus 2.0. Gut. 2024;73(2):361-371. DOI:10.1136/gutjnl-2023-330616
-6. Vakil N, Van Zanten SV, Kahrilas P, Dent J, Jones R, Bianchi LK, et al. The Montreal definition and classification of gastroesophageal reflux disease: A global evidence-based consensus. Am J Gastroenterol. 2006;101(8):1900-20.
-7. Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. ACG Clinical Guideline for the Diagnosis and Management of Gastroesophageal Reflux Disease. Am J Gastroenterol. 2022;117(1):27-56.
-8. Nguyen NT, Thosani NC, Canto M, Lipham J, Abu Dayyeh B, Wilson E, Muthusamy V, Clarke J, Bell R, Janu P, Swanstrom L, Runge A, Kahrilas PJ. The American Foregut Society White Paper on the Endoscopic Classification of Esophagogastric Junction Integrity. Foregut. 2022;2(4):1-12. DOI:10.1177/26345161221126961
-9. Yadlapati R, Kahrilas PJ, Fox MR, Bredenoord AJ, Gyawali CP, Roman S, et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0. Neurogastroenterol Motil. 2021;33(1):e14058. DOI:10.1111/nmo.14058
-10. Gyawali CP, Rogers BD, Frazzoni M, Savarino E, Sifrim D, Yadlapati R, et al. The role of high-resolution manometry in the evaluation of esophageal symptoms and disorders. Neurogastroenterol Motil. 2019;31(12):e13649. https://pmc.ncbi.nlm.nih.gov/articles/PMC6771035/
-11. Park S, Lee JH, Kim M, Lee S, Lee H, Yang H, et al. Exploring objective factors to predict successful outcomes after laparoscopic Nissen fundoplication. Int J Surg. 2023;109:299-305. DOI:10.1097/JS9.0000000000000451
-12. Olmos JA, Pandolfino JE, Piskorz MM, Zamora N, Valdovinos Díaz MA, Remes Troche JM, et al. Latin American consensus on diagnosis of gastroesophageal reflux disease. Neurogastroenterol Motil. 2024;36(5):e14735. DOI:10.1111/nmo.14735
-13. Gabbard S, Vijayvargiya S. Functional heartburn: An underrecognized cause of PPI-refractory symptoms. Cleve Clin J Med. 2019;86(12):799-806. DOI:10.3949/ccjm.86a.19006
-14. Yamasaki T, Sato H, Iwakiri K, et al. Reflux hypersensitivity: A new functional esophageal disorder. J Neurogastroenterol Motil. 2017;23(4):499-506. DOI:10.5056/jnm17097
-15. Carrott PW, Hong J, Kuppusamy M, Koehler RP, Low DE. Clinical ramifications of giant paraesophageal hernias are underappreciated: making the case for routine surgical repair. Ann Thorac Surg. 2012;94(2):421-426.
-16. Desjardin M, Luc G, Collet D, Zerbib F. 24-hour pH-impedance monitoring on therapy to select patients with refractory reflux symptoms for antireflux surgery. A single center retrospective study. Neurogastroenterol Motil. 2016;28(1):146-152. DOI:10.1111/nmo.12715
-17. Francis DO, Goutte M, Slaughter JC, et al. Traditional reflux parameters and not impedance monitoring predict outcome after fundoplication in extraesophageal reflux. Laryngoscope. 2011;121(9):1902-1909. DOI:10.1002/lary.21897
-18. Canon CL, Levine MS, Bryn S, et al. Society of Abdominal Radiology consensus statement for barium esophagography in gastroesophageal reflux disease. AJR Am J Roentgenol. 2016;206(6):1093-1103. DOI:10.2214/AJR.15.15754
-19. Nguyen AD, Carlson DA, Patel A, Gyawali CP. AGA Clinical Practice Update on Incorporating Functional Lumen Imaging Probe Into Esophageal Clinical Practice: Expert Review. Gastroenterology. 2025;169:726-736.
-20. Carlson DA, Pandolfino JE, Yadlapati R, Vela MF, Spechler SJ, Schnoll-Sussman FH, et al. A Standardized Approach to Performing and Interpreting Functional Lumen Imaging Probe Panometry for Esophageal Motility Disorders: The Dallas Consensus. Gastroenterology. 2025;168(6):1114-1127.e5. DOI:10.1053/j.gastro.2025.01.234
-21. Velanovich V. The development of the GERD-HRQL symptom severity instrument. Dis Esophagus. 2007;20(2):130-134. DOI:10.1111/j.1442-2050.2007.00658.x
-22. Rijnhart-De Jong HG, Draaisma WA, Smout AJ, Broeders IA, Gooszen HG. The Visick score: a good measure for the overall effect of antireflux surgery?. Scand J Gastroenterol. 2008;43(7):787-793. DOI:10.1080/00365520801935467
-23. Galmiche JP, Hatlebakk J, Attwood S, et al. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: the LOTUS randomized clinical trial. JAMA. 2011;305(19):1969-77. DOI:10.1001/jama.2011.626
-24. Du X, Hu Z, Yan C, Zhang C, Wang Z, Wu J. A meta-analysis of long follow-up outcomes of laparoscopic Nissen (total) versus Toupet (270°) fundoplication for gastro-esophageal reflux disease based on randomized controlled trials in adults. BMC Gastroenterol. 2016;16(1):88. DOI:10.1186/s12876-016-0502-8
-25. Bonavina L, Saino G, Lipham JC, Demeester TR. LINX® Reflux Management System in chronic gastroesophageal reflux: a novel effective technology for restoring the natural barrier to reflux. Ther Adv Gastroenterol. 2013;6(4):261-8. DOI:10.1177/1756283X13486311
-26. Bell RCW, Lipham JC, Louie BE, et al. Magnetic sphincter augmentation superior to proton pump inhibitors for regurgitation in a 1-year randomized trial. Clin Gastroenterol Hepatol. 2020;18(8):1736-1743.e2
-27. Alicuben ET, Bell RCW, Jobe BA, Buckley FP 3rd, Smith CD, Graybeal CJ, Lipham JC. Worldwide experience with erosion of the magnetic sphincter augmentation device. J Gastrointest Surg. 2018;22(9):1442-1447. DOI:10.1007/s11605-018-3775-0
-28. Aiolfi A, Asti E, Bernardi D, Bonitta G, Rausa E, Siboni S, Bonavina L. Early results of magnetic sphincter augmentation versus fundoplication for gastroesophageal reflux disease: systematic review and meta-analysis. Int J Surg. 2018;52:82-8. DOI:10.1016/j.ijsu.2018.02.034
-29. Telem D, et al. SAGES LINX® Safety and Effectiveness Analysis. SAGES TAVAC. 2021
-30. Janu P, Shoughoury AB, Venkat K, Hurwich D, Galouzis T, Siatras J, et al. Hybrid TIF: Laparoscopic Hiatal Hernia Repair (HHR) Followed Immediately by Transoral Incisionless Fundoplication (TIF) Using the EsophyX Device - Efficacy and Safety in 99 Patients in a Community Setting. Abstract No. 865
-31. Choi AY, Roccato MK, Samarasena JB, Kolb JM, Lee DP, Lee RH, Daly S, Hinojosa MW, Smith BR, Nguyen NT, Chang KJ. Novel Interdisciplinary Approach to GERD: Concomitant Laparoscopic Hiatal Hernia Repair with Transoral Incisionless Fundoplication. J Am Coll Surg. 2021;232(3):309-318. DOI:10.1016/j.jamcollsurg.2020.11.021. PMID:33346082
-32. Jaber F, Ayyad M, Ayoub F, Elhusseiny T, Abdelrahman A, Hammoud S, et al. Concomitant hiatal hernia repair with transoral incisionless fundoplication for the treatment of refractory gastroesophageal reflux disease: a systematic review. Surg Endosc. 2024;38(10):5528-5540. DOI:10.1007/s00464-024-11201-2
-33. Gergen AK, Wagh MS, Menard-Katcher P, Pratap A. Efficacy of Combined Hiatal Hernia Repair and Transoral Incisionless Fundoplication for Giant Paraoesophageal Hernias: Technique and Early Results. Surg Laparosc Endosc Percutan Tech. 2022;32(3):404-8
-34. Faria I, Isik A, Salem A, Piazzi F, Salem YH. Concomitant Transoral Incisionless Fundoplication Outcomes and Efficacy for Gastroesophageal Reflux Disease: A Retrospective Analysis. Am J Gastroenterol. 2022;117(10S):e779. DOI:10.14309/01.ajg.0000860936.27185.e8
-35. Forssell S, Bredenoord AJ. The RefluxStop™ device: safety and efficacy at 6-12 months. World J Surg. 2021;45(1):72-79
-36. Feka J, Saad M, Boyle N, Paireder M, Kristo I, Rieder E, Asari R, Schoppmann SF. Multicentric short term and safety study of ineffective esophageal motility patients treated with RefluxStop device. Sci Rep. 2024;14(1):15425. DOI:10.1038/s41598-024-65751-5
-37. Rodríguez L, Rodriguez P, Gómez B, Ayala JC, Oxenberg D, Perez-Castilla A, et al. Two-year results of intermittent electrical stimulation of the lower esophageal sphincter treatment of gastroesophageal reflux disease. Surgery. 2015;157(3):556-67
-38. Hoppo T, Rodríguez L, Soffer E, Crowell MD, Jobe BA. Long-term results of electrical stimulation of the lower esophageal sphincter for treatment of proximal GERD. Surg Endosc. 2014;28(12):3293-3301
-39. Duke MC, Farrell TM. Surgery for Gastroesophageal Reflux Disease in the Morbidly Obese Patient. J Laparoendosc Adv Surg Tech. 2016. DOI:10.1089/lap.2016.29013.mcd
-40. Pauwels A, Boecxstaens V, Andrews CN, et al. How to select patients for antireflux surgery? The ICARUS guidelines (international consensus regarding preoperative examinations and clinical characteristics assessment to select adult patients for antireflux surgery). Gut. 2019;68(11):1928-1941. DOI:10.1136/gutjnl-2019-318260
-41. Felsenreich DM, Kefurt R, Schermann M, Beckerhinn P, Kristo I, Krebs M, Prager G, Langer FB. Reflux, Sleeve Dilation, and Barrett’s Esophagus after Laparoscopic Sleeve Gastrectomy: Long-Term Follow-Up. Obes Surg. 2017. DOI:10.1007/s11695-017-2748-9
-42. Carroll R, Fontan F, Lehmann R, Smith J, Nau P. Laparoscopic Roux-en-Y gastric bypass for the management of hiatal hernia and failed fundoplication in patients with obesity. Ann Laparosc Endosc Surg. 2021;6:23. DOI:10.21037/ales-20-75
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2025 David Solinas, Mauricio Ramírez, Alejandro Nieponice

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.












