Sobrecrecimiento bacteriano del intestino delgado y sobrecrecimiento metanógeno intestinal: ¿están sobrediagnosticados?
DOI:
https://doi.org/10.52787/agl.v55i4.570Palabras clave:
Sobrecrecimiento bacteriano del intestino delgado, intestino delgado, malabsorción, microbioma, síndrome del intestino irritableResumen
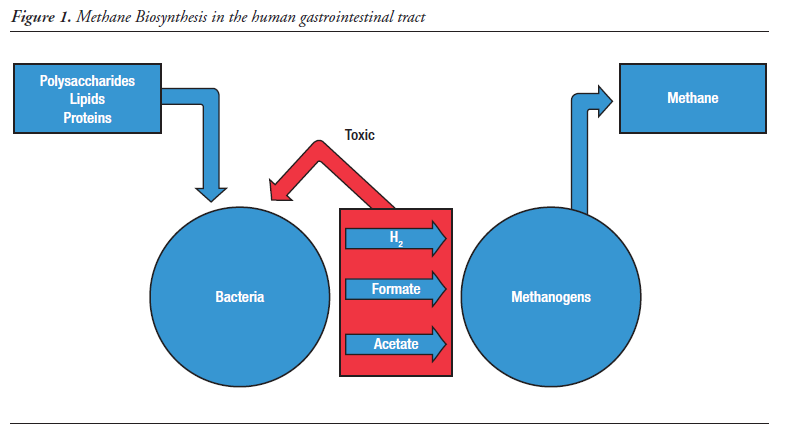
El sobrecrecimiento bacteriano del intestino delgado se describió originalmente como una causa de mala digestión y malabsorción, y su diagnóstico se basaba en el cultivo de aspirados del intestino delgado superior; sin embargo, la aplicación de pruebas de hidrógeno en el aliento para evaluar la sospecha de sobrecrecimiento bacteriano del intestino delgado aumentó drásticamente la frecuencia de este diagnóstico y amplió su contexto clínico desde la mala digestión hasta incluir una serie de molestias gastrointestinales inespecíficas e incluso algunas enfermedades sistémicas. No obstante, una revisión crítica de la literatura reciente sugiere que la dependencia de las pruebas de aliento, en particular aquellas que utilizan lactulosa como sustrato, ha llevado a un sobrediagnóstico del sobrecrecimiento bacteriano del intestino delgado, ya que muchos aspectos del concepto actual de su diagnóstico siguen siendo controvertidos y no resueltos, incluidos los umbrales diagnósticos, la respuesta al tratamiento con antibióticos y el papel del metano, el sulfuro de hidrógeno y otros gases derivados de la fermentación bacteriana en el tracto gastrointestinal. En este contexto, se analizan estos temas prestando especial atención al concepto de sobrecrecimiento de metanógenos intestinales y al papel de los metanógenos y el metano en la homeostasis gastrointestinal, se aboga por un enfoque crítico y cauteloso en el diagnóstico tanto del sobrecrecimiento bacteriano del intestino delgado como del sobrecrecimiento de metanógenos intestinales y por una gran prudencia en la prescripción de antibióticos, y se destaca el interés en la aplicación de la microbiología molecular moderna al estudio del microbioma y el metaboloma del intestino delgado, con el objetivo de lograr una comprensión más completa de la biología del metano.
Citas
-1. Chen TS, Chen PS. Intestinal autointoxication: a medical leitmotif. J Clin Gastroenterol. 1989;11:434-41.
-2. Card WI. Blind loop syndrome. Proc R Soc Med. 1959;52:28-31.
-3. Barker WH, Hummel LE. Macrocytic anemia in association with intestinal strictures and anastomosis – review of the literature and report of two new cases. Bull Johns Hopkins Hosp. 1939;64:215-56.
-4. Gracey M. Intestinal absorption in the “contaminated small-bowel syndrome”. Gut. 1971;12:403-10.
-5. Sherlock S, Summerskill WH, White LP, Phear EA. Portal-systemic encephalopathy; neurological complications of liver disease. Lancet. 1954;267:454-7.
-6. Bushyhead D, Quigley EMM. Small Intestinal Bacterial Overgrowth-Pathophysiology and Its Implications for Definition and Management. Gastroenterology. 2022;163:593-607.
-7. Quigley EM. Small intestinal bacterial overgrowth: from malabsorption to misinterpretation. Minerva Gastroenterol (Torino). 2025;71:65-73.
-8. Tabaqchali S, Okubadejo OA, Neale G, Booth CC. Influence of abnormal bacterial flora on small intestinal function. Proc R Soc Med. 1966;59:1244-6.
-9. King CE, Toskes PP, Guilarte TR, Lorenz E, Welkos SL. Comparison of the one-gram d-[14C]xylose breath test to the [14C] bile acid breath test in patients with small-intestine bacterial overgrowth. Dig Dis Sci. 1980;25:53-8.
-10. Bond JH, Levitt MD, Prentiss R. Investigation of small bowel transit time in man utilizing pulmonary hydrogen (H2) measurements. J Lab Clin Med. 1975;85:546-55.
-11. Pimentel M, Chow EJ, Lin HC. Eradication of small intestinal bacterial overgrowth reduces symptoms of irritable bowel syndrome. Am J Gastroenterol. 2000;95:3503-6.
-12. Pimentel M, Chow EJ, Lin HC. Normalization of lactulose breath testing correlates with symptom improvement in irritable bowel syndrome: a double-blind, randomized, placebo-controlled study. Am J Gastroenterol. 2003;98:412-9.
-13. Pimentel M, Lembo A, Chey WD, Zakko S, Ringel Y, Yu J, et al. Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med. 2011;364:22-32.
-14. Rezaie A, Heimanson Z, McCallum R, Pimentel M. Lactulose breath testing as a predictor of response to rifaximin in patients with irritable bowel syndrome with diarrhea. Am J Gastroenterol. 2019;114:1886-93.
-15. Yu D, Cheeseman F, Vanner S. Combined oro-caecal scintigraphy and lactulose hydrogen breath testing demonstrate that breath testing detects oro-caecal transit, not small intestinal bacterial overgrowth in patients with IBS. Gut. 2011;60:334-40.
-16. Ford AC, Spiegel BMR, Talley NJ, Moayyedi P. Small intestinal bacterial overgrowth in irritable bowel syndrome: systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2009;7:1279-86.
-17. Shah A, Talley NJ, Jones M, Kendall BJ, Koloski N, Walker MM, et al. Small intestinal bacterial overgrowth in irritable bowel syndrome: a systematic review and meta-analysis of case-control studies. Am J Gastroenterol. 2020;115:190-201.
-18. Kashyap P, Moayyedi P, Quigley EMM, Simren M, Vanner S. Critical appraisal of the SIBO hypothesis and breath testing: a clinical practice update endorsed by the ESNM and ANMS. Neurogastroenterol Motil. 2024;36:e14817.
-19. Lin EC, Massey BT. Scintigraphy demonstrates high rate of false-positive results from glucose breath tests for small bowel bacterial overgrowth. Clin Gastroenterol Hepatol. 2016;14:203-8.
-20. Shanahan ER, Zhong L, Talley NJ, Morrison M, Holtmann G. Characterisation of the gastrointestinal mucosa-associated microbiota: a novel technique to prevent cross-contamination during endoscopic procedures. Aliment Pharmacol Ther. 2016;43:1186-96.
-21. Karunaratne TB, Sharma A, Rao SSC. Small-bowel aspiration during upper esophagogastroduodenoscopy: Rao technique. VideoGIE. 2021;6:152-4.
-22. Li J, Zhang R, Ma J, Tang S, Li Y, Li Y, et al. Mucosa-associated microbial profile is altered in small intestinal bacterial overgrowth. Front Microbiol. 2021;12:710940.
-23. Shin AS, Gao X, Bohm M, Lin H, Gupta A, Nelson DE, et al. Characterization of proximal small intestinal microbiota in patients with suspected small intestinal bacterial overgrowth: a cross-sectional study. Clin Transl Gastroenterol. 2019;10:e00073.
-24. Saffouri GB, Shields-Cutler RR, Chen J, Yang Y, Lekatz HR, Hale VL, et al. Small intestinal microbial dysbiosis underlies symptoms associated with functional gastrointestinal disorders. Nat Commun. 2019;10:2012.
-25. Leite G, Morales W, Weitsman S, Celly S, Parodi G, Mathur R, et al. The duodenal microbiome is altered in small intestinal bacterial overgrowth. PLoS One. 2020;15:e0234906.
-26. Barlow JT, Leite G, Romano AE, Sedighi R, Chang C, Celly S, et al. Quantitative sequencing clarifies the role of disruptor taxa, oral microbiota, and strict anaerobes in the human small-intestine microbiome. Microbiome. 2021;9:214.
-27. Bamba S, Imai T, Sasaki M, Ohno M, Yoshida S, Nishida A, et al. Altered gut microbiota in patients with small intestinal bacterial overgrowth. J Gastroenterol Hepatol. 2023;38:61-9.
-28. Leite G, Rezaie A, Mathur R, Barlow GM, Rashid M, Hosseini A, et al. Defining Small Intestinal Bacterial Overgrowth by Culture and High Throughput Sequencing. Clin Gastroenterol Hepatol. 2024;22:259-70.
-29. Rezaie A, Buresi M, Lembo A, Lin H, McCallum R, Rao S, et al. Hydrogen and Methane-Based Breath Testing in Gastrointestinal Disorders: The North American Consensus. The American Journal of Gastroenterology. 2017;112:775.
-30. Read NW, Miles CA, Fisher D, Holgate AM, Kime ND, Mitchell MA, et al. Transit of a meal through the stomach, small intestine, and colon in normal subjects and its role in the pathogenesis of diarrhea. Gastroenterology. 1980;79:1276-82.
-31. Jiménez-Castillo RA, Félix-Téllez FA, Vargas-Basurto JL, Noriega-García NB, Suárez-Fernández M, García-Zermeño KR, et al. Diagnostic Reliability of Glucose and Lactulose Breath Tests: Insights From a Test-Retest Study in Healthy Adults. Neurogastroenterol Motil. 2025;e70089.
-32. Takakura W, Rezaie A, Chey WD, Wang J, Pimentel M. Symptomatic Response to Antibiotics in Patients With Small Intestinal Bacterial Overgrowth: A Systematic Review and Meta-analysis. J Neurogastroenterol Motil. 2024;30:7-16.
-33. Lauritano EC, Gabrielli M, Scarpellini E, Lupascu A, Novi M, Sottili S, et al. Small intestinal bacterial overgrowth recurrence after antibiotic therapy. Am J Gastroenterol. 2008;103:2031-5.
-34. Lembo A, Pimentel M, Rao SS, Schoenfeld P, Cash B, Weinstock LB, et al. Repeat Treatment With Rifaximin Is Safe and Effective in Patients With Diarrhea-Predominant Irritable Bowel Syndrome. Gastroenterology. 2016;151:1113-21.
-35. DuPont HL. The potential for development of clinically relevant microbial resistance to rifaximin-α: a narrative review. Clin Microbiol Rev. 2023;36:e00039-23.
-36. Turner AM, Li L, Monk IR, Lee JYH, Ingle DJ, Portelli S, et al. Rifaximin prophylaxis causes resistance to the last-resort antibiotic daptomycin. Nature. 2024;635:969-77.
-37. Boll L, Kern WV, Schuster S, Schultheiß M, Schneider C, Vavra M, et al. Frequent high-level rifaximin resistance in Escherichia coli associated with long-term treatment of patients with liver cirrhosis: a prospective, controlled study. Microbiol Spectr. 2025;13:e0334724.
-38. Pimentel M, Gunsalus RP, Rao SSC, Zhang H. Methanogens in Human Health and Disease. The American Journal of Gastroenterology Supplements. 2012;1:28-33.
-39. Triantafyllou K, Chang C, Pimentel M. Methanogens, Methane and Gastrointestinal Motility. J Neurogastroenterol Motil. 2014;20:31-40.
-40. Levitt MD, Furne JK, Kuskowski M, Ruddy J. Stability of Human Methanogenic Flora Over 35 Years and a Review of Insights Obtained From Breath Methane Measurements. Clin Gastroenterol Hepatol. 2006;4:123-9.
-41. Florin THJ, Zhu G, Kirk KM, Martin NG. Shared and unique environmental factors determine the ecology of methanogens in humans and rats. Am J Gastroenterol. 2000;95:2872-9.
-42. Kumpitsch C, Fischmeister FPhS, Mahnert A, Lackner S, Wilding M, Sturm C, et al. Reduced B12 uptake and increased gastrointestinal formate are associated with archaeome-mediated breath methane emission in humans. Microbiome. 2021;9:193.
-43. Hansen EE, Lozupone CA, Rey FE, Wu M, Guruge JL, Narra A, et al. Pan-genome of the dominant human gut-associated archaeon, Methanobrevibacter smithii, studied in twins. Proc Natl Acad Sci U S A. 2011;108(Suppl 1):4599-606.
-44. Hoegenauer C, Hammer HF, Mahnert A, Moissl-Eichinger C. Methanogenic archaea in the human gastrointestinal tract. Nat Rev Gastroenterol Hepatol. 2022;19:805-13.
-45. Min YW, Rezaie A, Pimentel M. Bile Acid and Gut Microbiota in Irritable Bowel Syndrome. J Neurogastroenterol Motil. 2022;28:549-61.
-46. An C, Chon H, Ku W, Eom S, Seok M, Kim S, et al. Bile Acids: Major Regulator of the Gut Microbiome. Microorganisms. 2022;10:1792.
-47. Florin TH, Jabbar IA. A possible role for bile acid in the control of methanogenesis and the accumulation of hydrogen gas in the human colon. J Gastroenterol Hepatol. 1994;9:112-7.
-48. Djemai K, Drancourt M, Tidjani Alou M. Bacteria and Methanogens in the Human Microbiome: a Review of Syntrophic Interactions. Microb Ecol. 2022;83:536-54.
-49. Fiedorek SC, Pumphrey CL, Casteel HB. Breath methane production in children with constipation and encopresis. J Pediatr Gastroenterol Nutr. 1990;10:473-7.
-50. Pimentel M, Mayer AG, Park S, Chow EJ, Hasan A, Kong Y. Methane production during lactulose breath test is associated with gastrointestinal disease presentation. Dig Dis Sci. 2003;48:86-92.
-51. Chatterjee S, Park S, Low K, Kong Y, Pimentel M. The Degree of Breath Methane Production in IBS Correlates With the Severity of Constipation. Am J Gastroenterol. 2007;102:837.
-52. Mehravar S, Takakura W, Wang J, Pimentel M, Nasser J, Rezaie A. Symptom Profile of Patients With Intestinal Methanogen Overgrowth: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2025;23:1111-1122.e9.
-53. Pimentel M, Lin HC, Enayati P, van den Burg B, Lee HR, Chen JH, et al. Methane, a gas produced by enteric bacteria, slows intestinal transit and augments small intestinal contractile activity. Am J Physiol Gastrointest Liver Physiol. 2006;290:G1089-95.
-54. Jahng J, Jung IS, Choi EJ, Conklin JL, Park H. The effects of methane and hydrogen gases produced by enteric bacteria on ileal motility and colonic transit time. Neurogastroenterol Motil. 2012;24:185-e92.
-55. Attaluri A, Jackson M, Valestin J, Rao SS. Methanogenic Flora Is Associated With Altered Colonic Transit but Not Stool Characteristics in Constipation Without IBS. Am J Gastroenterol. 2010;105:1407.
-56. Talamantes S, Steiner F, Spencer S, Neshatian L, Sonu I. Intestinal Methanogen Overgrowth (IMO) Is Associated with Delayed Small Bowel and Colonic Transit Time on the Wireless Motility Capsule. Dig Dis Sci. 2024;69:3361-8.
-57. Procházková N, Falony G, Dragsted LO, Licht TR, Raes J, Roager HM. Advancing human gut microbiota research by considering gut transit time. Gut. 2023;72:180-91.
-58. Tottey W, Feria-Gervasio D, Gaci N, Laillet B, Pujos E, Martin JF, et al. Colonic Transit Time Is a Driven Force of the Gut Microbiota Composition and Metabolism: In Vitro Evidence. J Neurogastroenterol Motil. 2017;23:124-34.
-59. El Oufir L, Flourié B, Bruley des Varannes S, Barry JL, Cloarec D, Bornet F, et al. Relations between transit time, fermentation products, and hydrogen consuming flora in healthy humans. Gut. 1996;38:870-7.
-60. Kim G, Deepinder F, Morales W, Hwang L, Weitsman S, Chang C, et al. Methanobrevibacter smithii Is the Predominant Methanogen in Patients with Constipation-Predominant IBS and Methane on Breath. Dig Dis Sci. 2012;57:3213-8.
-61. Di Stefano M, Mengoli C, Bergonzi M, Klersy C, Pagani E, Miceli E, et al. Breath Methane Excretion Is not An Accurate Marker of Colonic Methane Production in Irritable Bowel Syndrome. Official journal of the American College of Gastroenterology | ACG. 2015;110:891.
-62. Pimentel M, Constantino T, Kong Y, Bajwa M, Rezaei A, Park S. A 14-Day Elemental Diet Is Highly Effective in Normalizing the Lactulose Breath Test. Dig Dis Sci. 2004;49:73-7.
-63. O’Dwyer D. Homemade Elemental Diet to Treat Intestinal Methanogen Overgrowth: A Case Report. Integr Med (Encinitas). 2021;20:32–41.
-64. Eetemadi A, Tagkopoulos I. Methane and fatty acid metabolism pathways are predictive of Low-FODMAP diet efficacy for patients with irritable bowel syndrome. Clin Nutr. 2021;40:4414-21.
-65. Dridi B, Fardeau ML, Ollivier B, Raoult D, Drancourt M. The antimicrobial resistance pattern of cultured human methanogens reflects the unique phylogenetic position of archaea. J Antimicrob Chemother. 2011;66:2038-44.
-66. Pimentel M, Chatterjee S, Chow EJ, Park S, Kong Y. Neomycin Improves Constipation-Predominant Irritable Bowel Syndrome in a Fashion That Is Dependent on the Presence of Methane Gas: Subanalysis of a Double-Blind Randomized Controlled Study. Dig Dis Sci. 2006;51:1297-301.
-67. Ghoshal UC, Srivastava D, Verma A, Misra A. Slow Transit Constipation Associated With Excess Methane Production and Its Improvement Following Rifaximin Therapy: A Case Report. J Neurogastroenterol Motil. 2011;17:185-8.
-68. Ojetti V, Ianiro G, Tortora A, D’Angelo G, Di Rienzo TA, Bibbò S, et al. The effect of Lactobacillus reuteri supplementation in adults with chronic functional constipation: a randomized, double-blind, placebo-controlled trial. J Gastrointestin Liver Dis. 2014;23:387-91.
-69. Ojetti V, Petruzziello C, Migneco A, Gnarra M, Gasbarrini A, Franceschi F. Effect of Lactobacillus reuteri (DSM 17938) on methane production in patients affected by functional constipation: a retrospective study. Eur Rev Med Pharmacol Sci. 2017;21.
-70. Gottlieb K, Wacher V, Sliman J, Pimentel M. Review article: inhibition of methanogenic archaea by statins as a targeted management strategy for constipation and related disorders. Aliment Pharmacol Ther. 2016;43:197-212.
-71. Demonfort Nkamga V, Armstrong N, Drancourt M. In vitro susceptibility of cultured human methanogens to lovastatin. Int J Antimicrob Agents. 2017;49:176-82.
-72. Scheithauer TPM, Dallinga-Thie GM, De Vos WM, Nieuwdorp M, Van Raalte DH. Causality of small and large intestinal microbiota in weight regulation and insulin resistance. Mol Metab. 2016;5:759-70.
-73. Kuang J, Zheng X, Jia W. Investigating regional-specific gut microbial distribution: an uncharted territory in disease therapeutics. Protein Cell. 2025;16:623-40.
-74. Booijink CCGM, Zoetendal EG, Kleerebezem M, de Vos WM. Microbial communities in the human small intestine: coupling diversity to metagenomics. Future Microbiol. 2007;2:285-95.
-75. Zheng L, Kelly CJ, Colgan SP. Physiologic hypoxia and oxygen homeostasis in the healthy intestine. Am J Physiol Cell Physiol. 2015;309:C350-60.
-76. He G, Shankar RA, Chzhan M, Samouilov A, Kuppusamy P, Zweier JL. Noninvasive measurement of anatomic structure and intraluminal oxygenation in the gastrointestinal tract of living mice with spatial and spectral EPR imaging. Proc Natl Acad Sci U S A. 1999;96:4586-91.
-77. Fisher EM, Khan M, Salisbury R, Kuppusamy P. Noninvasive monitoring of small intestinal oxygen in a rat model of chronic mesenteric ischemia. Cell Biochem Biophys. 2013;67:10.1007/s12013-013-9611-y.
-78. Konjar Š, Pavšič M, Veldhoen M. Regulation of Oxygen Homeostasis at the Intestinal Epithelial Barrier Site. Int J Mol Sci. 2021;22:9170.
-79. Albenberg L, Esipova TV, Judge CP, Bittinger K, Chen J, Laughlin A, et al. Correlation Between Intraluminal Oxygen Gradient and Radial Partitioning of Intestinal Microbiota. Gastroenterology. 2014;147:1055-1063.e8.
-80. Singhal R, Shah YM. Oxygen battle in the gut: Hypoxia and hypoxia-inducible factors in metabolic and inflammatory responses in the intestine. J Biol Chem. 2020;295:10493-505.
-81. Villanueva-Millan MJ, Leite G, Mathur R, Rezaie A, Fajardo CM, de Freitas Germano J, et al. Hydrogen Sulfide and Methane on Breath Test Correlate with Human Small Intestinal Hydrogen Sulfide Producers and Methanogens. Dig Dis Sci. 2025 [epub ahead of print].
-82. Jensen BB, Jørgensen H. Effect of dietary fiber on microbial activity and microbial gas production in various regions of the gastrointestinal tract of pigs. Appl Environ Microbiol. 1994;60:1897-904.
-83. Yilmaz B, Macpherson AJ. Delving the depths of “terra incognita” in the human intestine – the small intestinal microbiota. Nat Rev Gastroenterol Hepatol. 2025;22:71-81.
-84. Zhu W, Zhang X, Wang D, Yao Q, Ma GL, Fan X. Simulator of the Human Intestinal Microbial Ecosystem (SHIME®): Current Developments, Applications, and Future Prospects. Pharmaceuticals (Basel). 2024;17:1639.
-85. Venema K, van den Abbeele P. Experimental models of the gut microbiome. Best Pract Res Clin Gastroenterol. 2013;27:115-26.
-86. Rossi R, Mainardi E. Prebiotics and Probiotics Supplementation in Pigs as a Model for Human Gut Health and Disease. Biomolecules. 2025;15:665.
-87. Wang M, Donovan SM. Human Microbiota-Associated Swine: Current Progress and Future Opportunities. ILAR J. 2015;56:63-73.
-88. van Trijp MP, Wilms E, Ríos-Morales M, Masclee AA, Brummer RJ, Witteman BJ, et al. Using naso- and oro-intestinal catheters in physiological research for intestinal delivery and sampling in vivo: practical and technical aspects to be considered. Am J Clin Nutr. 2021;114:843-61.
-89. Marquez-Ortiz RA, Leon M, Abril D, Escobar-Perez J, Florez-Sarmiento C, Parra-Izquierdo V, et al. Colonoscopy aspiration lavages for mucosal metataxonomic profiling of spondylarthritis-associated gastrointestinal tract alterations. Sci Rep. 2023;13:7015.
-90. Zoetendal EG, Raes J, van den Bogert B, Arumugam M, Booijink CC, Troost FJ, et al. The human small intestinal microbiota is driven by rapid uptake and conversion of simple carbohydrates. ISME J. 2012;6:1415-26.
-91. Nejati S, Wang J, Sedaghat S, Balog NK, Long AM, Rivera UH, et al. Smart Capsule for Targeted Proximal Colon Microbiome Sampling. Acta Biomater. 2022;154:83-96.
-92. Rehan M, Al-Bahadly I, Thomas DG, Young W, Cheng LK, Avci E. Smart capsules for sensing and sampling the gut: status, challenges and prospects. Gut. 2024;73:186-202.
-93. Stine JM, Ruland KL, Beardslee LA, Levy JA, Abianeh H, Botasini S, et al. Miniaturized Capsule System Toward Real-Time Electrochemical Detection of H2S in the Gastrointestinal Tract. Adv Healthc Mater. 2024;13:2302897.
-94. Berean KJ, Ha N, Ou JZ, Chrimes AF, Grando D, Yao CK, et al. The safety and sensitivity of a telemetric capsule to monitor gastrointestinal hydrogen production in vivo in healthy subjects: a pilot trial comparison to concurrent breath analysis. Aliment Pharmacol Ther. 2018;48:646-54.
-95. Shalon D, Culver RN, Grembi JA, Folz J, Treit PV, Shi H, et al. Profiling the human intestinal environment under physiological conditions. Nature. 2023;617:581-91.
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2025 Anokhi S Kholwadwala, Eamonn Quigley

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.












