Prevalence of Malnutrition in Patients with Liver Cirrhosis: Observational Study
DOI:
https://doi.org/10.52787/agl.v52i4.265Keywords:
Malnutrition, nutritional status, nutritional assessment, liver cirrhosis, nutritionAbstract
Introduction. Malnutrition is a frequent entity in patients with liver cirrhosis and has a negative impact on mortality.
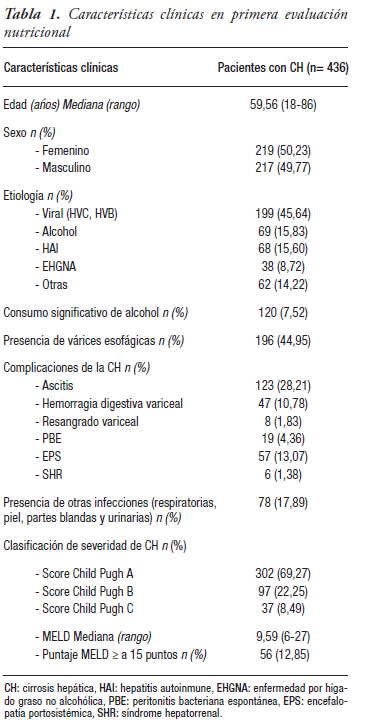
Aim. To describe the prevalence of malnutrition by means of subjective global assessment and anthropometry in patients with liver cirrhosis, and to analyze its relationship with the severity and etiology of the disease. Methods. We included patients > 18 years with liver cirrhosis, ambulatory or hospitalized, consecutively between May 2016 and April 2019; they underwent nutrition evaluation through subjective global assessment and anthropometry. Muscle strength was measured by dynamometry. Child-Pugh and MELD severity scores were evaluated. Statistical analysis: Chi-square test or Fisher's exact test and Mann-Whitney test. The statistical significance value was p <0.05.
Results. A total of 436 patients (50.2% women) were evaluated, age 59.6 ± 13 years, CP A 69.3%, B 22.2% and C 8.5%, MELD ≥15 points 12.8%. subjective global assessment and anthropometry were normal in 46.3% of the cases. The absolute concordance between subjective global assessment and anthropometry was 59.2% (kappa = 0.25); 49.5% of the patients presented some degree of malnutrition by subjective global assessment and 26.1% by anthropometry. This condition was diagnosed by aforementioned assessment in 36.1%, 77.3%, 86.5% in CP A, B and C, respectively, while by anthropometry, malnutrition was diagnosed in 20.5% of those with CP A, in 33% with CP B and in 54% with CP C. A significant association was also found according to the MELD score by anthropometry and subjective global assessment (p < 0.0001). Patients with alcoholic etiology presented greater malnutrition.
Conclusion. Malnutrition is common in patients with liver cirrhosis, with a high prevalence in compensated patients. The concordance between subjective global assessment and anthropometry was low, so the complementary use of subjective and objective tools would be convenient. Early detection of malnutrition would allow timely intervention.
References
-1. Schuppan D, Afdhal NH. Liver cirrhosis. Lancet [Internet]. 2008;371(9615):838-51.
-2. D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: A systematic review of 118 studies. J Hepatol [Internet]. 2006;44(1):217-31.
-3. Tsochatzis EA, Bosch J, Burroughs AK. Liver cirrhosis. Lancet [Internet]. 014;383(9930):1749-61.
-4. Bunchorntavakul C, Reddy KR. Review article: malnutrition/sarcopenia and frailty in patients with cirrhosis. Vol. 51, Alimentary Pharmacology and Therapeutics, pp. 64-77. Blackwell Publishing Ltd. 2020.
-5. Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr. 2017;36(1):49-64.
-6. Lochs H, Allison SP, Meier R, Pirlich M, Kondrup J, Schneider S, et al. Introductory to the ESPEN Guidelines on Enteral Nutrition: Terminology, Definitions and General Topics. Clin Nutr. 2006;25(2):180-6.
-7. Maharshi S, Sharma BC, Srivastava S. Malnutrition in cirrhosis increases morbidity and mortality. J Gastroenterol Hepatol. 2015;30(10):1507-13.
-8. Lai JC, Tandon P, Bernal W, Tapper EB, Ekong U, Dasarathy S, et al. Malnutrition, Frailty, and Sarcopenia in Patients with Cirrhosis: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology [Internet]. 2021;74(3):1611-44.
-9. Plauth M, Bernal W, Dasarathy S, Merli M, Plank LD, Schütz T, et al. ESPEN guideline on clinical nutrition in liver disease. Clin Nutr [Internet]. 2019;38(2):485-521.
-10. Gokturk HS, Selcuk H. Importance of malnutrition in patients with cirrhosis. Turkish J Gastroenterol [Internet]. 2015;26(4):291-6.
-11. Hanai T, Shiraki M, Nishimura K, Ogiso Y, Imai K, Suetsugu A, et al. Nutritional assessment tool for predicting sarcopenia in chronic liver disease. JCSM Rapid Commun. 2021;4(2):150-8.
-12. Cirrhosis IMCP on nutrition in liver. Nutritional status in cirrhosis. J Hepatol. 1994;21(7):317.
-13. Merli M, Berzigotti A, Zelber-Sagi S, Dasarathy S, Montagnese S, Genton L, et al. EASL Clinical Practice Guidelines on nutrition in chronic liver disease. J Hepatol [Internet]. 2019;70(1):172-93.
-14. Anand AC. Nutrition and Muscle in Cirrhosis. J Clin Exp Hepatol [Internet]. 2017;7(4):340-57.
-15. Merli M, Berzigotti A, Zelber-Sagi S, Dasarathy S, Montagnese S, Genton L, et al. EASL Clinical Practice Guidelines on nutrition in chronic liver disease. J Hepatol. 2019;70(1):172-93.
-16. Williams FR, Milliken D, Lai JC, Armstrong MJ. Assessment of the Frail Patient with End-Stage Liver Disease: A Practical Overview of Sarcopenia, Physical Function, and Disability. Hepatol Commun. 2021;5(6):923-37.
-17. Alberino F, Gatta A, Amodio P, Merkel C, Pascoli L Di, Boffo G, et al. Nutrition and Survival in Patients With Liver Cirrhosis. Nutrition. 2001;17(6):445-50.
-18. Tandon P, Low G, Mourtzakis M, Zenith L, Myers RP, Abraldes JG, et al. A Model to Identify Sarcopenia in Patients with Cirrhosis. Clin Gastroenterol Hepatol [Internet]. 2016;14(10):1473-1480.e3.
-19. Detsky AS, Mclaughlin JR, Baker JP, Johnston N, Whittaker S, Mendelson RA, et al. What is Subjective Global Assessment of Nutritional Status? 1987;11.
-20. Frisancho AR. New norms of upper limb fat and muscle areas for assessment of nutritional status. Am J Clin Nutr. 1981;34(11):2540-5.
-21. Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16-31.
-22. Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology 2003;124(1):91-6.
-23. Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60(8):646-9
-24. Angeli P, Bernardi M, Villanueva C, Francoz C, Mookerjee RP, Trebicka J, et al. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69(2):406-60.
-25. Montano-Loza AJ. Clinical relevance of sarcopenia in patients with cirrhosis. World J Gastroenterol. 2014;20(25):8061-71.
-26. Mazurak VC, Tandon P, Montano-Loza AJ. Nutrition and the Transplant Candidate. Liver Transplant [Internet]. 2017;23:1451-64.
-27. Merli M, Riggio O, Dally L. Does Malnutrition Affect Survival in Cirrhosis? Hepatology. 1996;23(5):1941-6.
-28. Morgan MY, Madden AM, Soulsby CT, Morris RW. Derivation and validation of a new global method for assessing nutritional status in patients with cirrhosis. Hepatology. 2006;44(4):823-35.
-29. Ferreira LG, Anastácio LR, Lima AS, Correia MITD. Assessment of nutritional status of patients waiting for liver transplantation. Clin Transplant. 2011;25(2):248-54.
-30. Ebadi M, Bhanji RA, Tandon P, Mazurak V, Baracos VE, Montano- Loza AJ. Review article: prognostic significance of body composition abnormalities in patients with cirrhosis. Aliment Pharmacol Ther. 2020;52(4):600-18.
-31. Campillo B, Richardet JP, Bores PN. Validation of body mass index for the diagnosis of malnutrition in patients with liver cirrhosis. Gastroenterol Clin Biol. 2006;30(10):1137-43.
-32. Ayala-Valverde, M., Arnold, J., Díaz, L.A. et al. Nutrition in Alcohol-Related Liver Disease. Curr Hepatology Rep. 2022; Supp 1:111–119.
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 María Cielo Gutiérrez, Andrea Curia, Enzo Rey, Juan Antonio Sordá, Jorge Daruich, Esteban González Ballerga

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.












