Chronic Atrophic Gastritis in Hispanics Treated at a Second-Level Hospital: Results of a Retrospective and Single-Center Study
DOI:
https://doi.org/10.52787/agl.v55i1.474Keywords:
Chronic atrophic gastritis, endoscopy, histologyAbstract
Introduction. The prevalence of chronic atrophic gastritis and intestinal metaplasia based on samples from third-level hospitals, may overestimate their frequency.
Objetive. To estimate the frequency of premalignant histological lesions of the stomach in a second-level hospital.
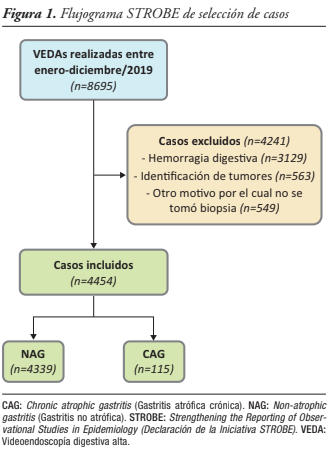
Material and methods. Observational, retrospective, descriptive, cross-sectional, epidemiological study. It was conducted with patients who had already undergone diagnostic upper digestive endoscopy, regardless of the clinical reason. Patients with gastrointestinal bleeding, tumors or without biopsy were excluded.
Results. A total of 4454 cases were reviewed, of which 115 (2.6%, CI 2.2 - 3.1) had chronic atrophic gastritis. Compared to non-atrophic gastritis, the presence of chronic atrophic gastritis was more frequent in older adults (43.5% vs. 24.9%; p < 001) and in those with dyspepsia symptoms (35.7% vs. 19.9%; p < 0.001); and less frequent in economically active population (47.8% vs. 64.9%; p < 0.001). Among patients with chronic atrophic gastritis, nearly twice as many tested positive for Helicobacter pylori (47.8% vs. 25.6%; p < 0.001). Helicobacter pylori infection nearly tripled the risk of developing chronic atrophic gastritis (Odds Ratio 2.65; p < 0.001).
Conclusion. In a second-level hospital, the prevalence of premalignant histological lesions is significantly lower than that reported by local studies conducted in third-level hospitals. The presence of chronic atrophic gastritis was associated with older age, indication for upper digestive endoscopy for dyspepsia, and Helicobacter pylori infection; while the indication for regurgitation was associated with its absence.
References
-1. Quinto R. Registro de Tumores Solca Matriz 2017. Rev Oncologia Ecu. 2017.
-2. Konturek PC, Brzozowski T, Konturek SJ, Kwiecień S, Pajdo R, Drozdowicz D, et al. Functional and morphological aspects of Helicobacter pylori-induced gastric cancer in Mongolian gerbils. Eur J Gastroenterol Hepatol. 2003;15(7):745-54.
-3. Ruiz B, Garay J, Johnson W, Li D, Rugge M, Dixon MF, et al. Morphometric assessment of gastric antral atrophy: Comparison with visual evaluation. Histopathology. 2001;39(3):235-42.
-4. Robles-Medranda C, Puga-Tejada M, Ospina J, Soria-Alcívar M, Bravo-Velez G, del Valle R, et al. Grading Atrophic Gastritis by a New Quantitative Method Using Confocal LASER Endomicroscopy Probe (P-CLE): First Resultas of a Prospective Cohort Study. Gastrointest Endosc [Internet]. 2015;81(5):AB464. Availablefrom: http://dx.doi.org/10.1016/j.gie.2015.03.1670
-5. Vásquez Buitrón PC, Febres-Cordero R. Prevalencia de infección por Helicobacter pylori y asociación con patologías gástricas en pacientes adultos de chequeo ejecutivo desde enero del 2010 hasta septiembre del 2012 del Hospital Metropolitano de Quito-Ecuador. [Quito-Ecuador]; 2013.
-6. Barreno Robalino RC, Abarca Ruíz JW. Validación de la relación pepsinógeno I/pepsinógeno II como test de screening en sujetos con atrofia gástrica. [Quito-Ecuador]; 2018.
-7. Guevara Aguirre MC, Guthemberg Morillo AA. Correlación del tratamiento farmacológico erradicador del Helicobacter pylori respecto a los cambios histopatológicos de la mucosa gástrica. [Quito-Ecuador]; 2014.
-8. Núñez Acurio DK, Escalante Vanoni S. Detección de los genesvacA y cagA en cepas de Helicobacter pylori obtenidas de un hospital de la ciudad de Quito y su asociación con el grado de lesión gástrica. [Quito-Ecuador]; 2017.
-9. Guamán-Guamán MI, Abarca-Ruíz JW. Validación endoscópica de la cromoendoscopía virtual (FICE) en la detección de lesiones preneoplásicas gástricas vs histopatología. [Quito-Ecuador]; 2018.
-10. Yo HP, Nayoung K. Review of Atrophic Gastritis and Intestinal Metaplasia as a Premalignant Lesion of Gastric Cancer. J Cancer Prev [Internet]. 2015 [cited 2020 Apr 28];20(1):25-2015. Available from: www.jcpjournal.org - https://www.jcpjournal.org/journal/view.html?doi=10.15430/JCP.2015.20.1.25
-11. Pimentel-Nunes P, Libânio D, Marcos-Pinto R, Areia M, Leja M, Esposito G, et al. Management of epithelial precancerous conditions and lesions in the stomach (MAPS II): European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter and Microbiota Study Group (EHMSG), European Society of Pathology (ESP), and Sociedade Port. Endoscopy. 2019;51(4):365-88.
-12. Robles-Medranda C, Vargas M, Ospina J, Puga-Tejada M, Valero M, Soria M, et al. Clinical impact of confocal laser endomicroscopy in the management of gastrointestinal lesions with an uncertain diagnosis. World J Gastrointest Endosc. 2017;9(8):389.
-13. Dixon MF, Genta RM, Yardley JH, Correa P, Batts KP, Dahms BB, et al. Classification and grading of Gastritis: The updated Sydney system. Am J Surg Pathol. 1996 Oct;20(10):1161-81.
-14. Crafa P, Russo M, Miraglia C, Barchi A, Moccia F, Nouvenne A, et al. From Sidney to OLGA: an overview of atrophic gastritis. Acta Biomed [Internet]. 2018 [cited 2020 Apr 15];89(Supplement 8):93-9. Availablefrom: www.actabiomedica.it
-15. Robles-Medranda C, Valero M, Puga-Tejada M, Oleas R, Baquerizo-Burgos J, Soria-Alcívar M, et al. High-definition optical magnification with digital chromoendoscopy detects gastric mucosal changes in dyspeptic-patients. World J Gastrointest Endosc. 2020;12(1):23-32.
-16. Zhao T, Liu F, Li Y. Effects of Helicobacter pylori eradication on esophageal motility, esophageal acid exposure, and gastroesophageal reflux disease symptoms. Front Cell Infect Microbiol. 2023 Mar 8;13:1082620.
-17. Lee YY, Prakash H, Talebi A, Abadi B, Iijima K, Koike T, et al. Reflux esophagitis triggered after Helicobacter pylori eradication: a noteworthy demerit of eradication therapy among the Japanese? Front Microbiol [Internet]. 2015 [cited 2025 Mar 15];6(JUN):566. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC4460561/
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Leysi Carvache, John Daluz, Andrés Pereira-Reinosa, Kléber Coppiano, Byron Bermeo, Alberto Campodónico, Miguel Puga-Tejada

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.












